The Ted Cruz plan that would send us back to the bad old days of American health insurance
A decade ago I interviewed a Florida woman who was the victim of the kind of egregious health insurance abuses that finally disappeared with the Affordable Care Act. They could surface again if the Republicans succeed with the latest health reform proposal offered by Texas Sen. Ted Cruz, which would result in a two-track insurance market. Insurers would be able to offer skimpy, low-cost policies that don’t cover much for people who don’t need much, while still being required to sell at least one broader plan offering all the ACA’s essential benefits to those with money enough to buy it.
The story of the Florida woman is instructive as Congress prepares to rip apart Obamacare, and return to the bad old days of America’s individual insurance market, where death spirals and a practice called “re-underwriting” or checking up on policyholders’ health each year were common. Insurers often purged policyholders who got sick because they were costly and an impediment to keeping stock prices high for investors. In the early 2000s, an official of the American Academy of Actuaries argued carriers should do more re-underwriting. He told The Wall Street Journal, “If regulators can overcome their emotional reaction and allow it to happen, I think it could be a useful tool in managing health care costs.”
The woman and her husband had bought a policy in the early 1990s from a small insurer. The monthly premium of $153 seemed about right. A few years later at age 46 she was diagnosed with breast cancer and their premium rose to $417. It kept climbing. By the late 1990s it reached nearly $600 for their two policies, and the company threatened to cancel her policy, which was in what insurers call “a block of business” that happened to be experiencing a death spiral. People were getting sicker, premiums were getting higher, healthy people were leaving, and the carrier wanted to close off the block and send the remaining customers elsewhere. One place was to an “association” connected to the insurer. The insurer would sell an association policy if the woman and others paid a $5 fee to belong to the group. Desperate, she and her husband paid, but her monthly premium doubled, to $1,180 with a $500 deductible, high for those days.
What’s likely to happen should the Cruz plan gain traction and make it into a final Senate bill? Sick people will still opt for more expensive coverage and healthy people will take their chances on the cheapie plans.
When it reached $1,900 in 2000, they demanded to know why and drove 1,500 miles to the insurer’s home office. They were told that each year the company evaluated her as if she was a new person applying for coverage. They also said that policyholders such as themselves were dumped into three buckets. Those with few claims got rate increases based only on medical inflation; those in the second group who had some health problems got increases based on inflation plus 5 percent; while people with heart disease or cancer like the woman could expect premium increases of 37 percent that year, plus the normal raise for inflation. Company officials told her to expect rate hikes like that in the future “because of your dread disease.”
Most of the 19 million Americans buying coverage in the individual insurance market today, both on and off the state insurance exchanges, surely would not want to return to that kind of marketplace. So far, I’d bet most of them are in the dark about what might happen to them. They need to be better informed on how things could change for them if the Cruz plan is part of a final legislation the Senate might pass. They need to know and understand more than what was in an Associated Press story Tuesday, which simply reported:
Cruz has proposed letting insurers sell any policy they’d like, as long as they also sell one that covers a list of services like maternity care that Obama’s law requires. The Cruz amendment was alienating senators like Collins amid concerns it would lead to unaffordable prices for people with preexisting medical conditions because younger, healthier customers wouldn’t be sharing their costs.
The ACA health insurance markets are shaky enough without new rules that could make some of them crumble altogether. Only 40 percent of Americans eligible for an Obamacare policy signed up for one this year. Many of those who did were ill and needed the coverage. People in good health didn’t join, which weakened the risk pool and raised premiums in some parts of the country even more. This year many carriers have left those markets, and next year there will be even fewer. It’s not good business for them. The Centers for Medicare and Medicaid Services just announced that that the number of sellers will drop by a more than a third.
What’s likely to happen should the Cruz plan gain traction and make it into a final Senate bill? Sick people will still opt for more expensive coverage and healthy people will take their chances on the cheapie plans. That sort of sounds like the buckets of policyholders the Florida woman’s insurance company had set up, before dumping her in the high-priced pail. Cruz explained his plan Sunday on ABC’s “This Week”: “The question really is here is how are we going to provide for, how are we going to provide assistance to people with serious diseases, serious pre-existing conditions. There’s widespread agreement in Congress there’s going to be significant assistance.”
The Senate bill calls for a $100 billion fund to help hold down premiums. But given how fast health costs grow as more new technology comes on the market, coupled with the bill’s lack of measures to curb health care costs, what happens when the money runs out or is insufficient to help all the people who need it? Who will pay for their care? Or will they go without?
There’s only one way to make sure this doesn’t happen — get everyone into the risk pool together, which is what Medicare does and national insurance systems in other countries do. But neither Congress nor the Republicans are moving in this direction. So if Cruz’s ideas make it to the finish line, we may be stuck for the time being with the Florida woman’s dilemma.
Like all tales her story has an ending, one with implications for what might pass Congress in the next few weeks. There was little regulation of insurers’ association policies in Florida at the time and even less in Ohio where the association’s master policy was filed. So she worked with legislators to toughen Florida’s regulations for individual market policies. There, she told me, she learned how legislation really gets passed. “I was naïve,” she said. “I thought you go up there and testify and the laws would get changed. Insurance lobbyists descended on Tallahassee and stopped the bill cold.”
After a few years of legislative wrangling, a watered-down bill did pass, which curbed some of the worst market abuses she encountered. But, she added, “It was very, very evident legislators were going to do what the special interest groups said.”
We’re still waiting to see who’s behind the Cruz proposal. Which insurance companies will benefit from the new market for stripped down insurance his proposal would create? The Blue Cross Blue Shield Association and the industry group America’s Health Insurance Plans both said this week they don’t support the Cruz amendment. But that doesn’t necessarily mean all carriers agree. Some insurers could get a huge windfall here by bringing back barebones catastrophic plans.
Veteran health care journalist Trudy Lieberman is a contributing editor at the Center for Health Journalism Digital and a regular contributor to the Remaking Health Care blog.
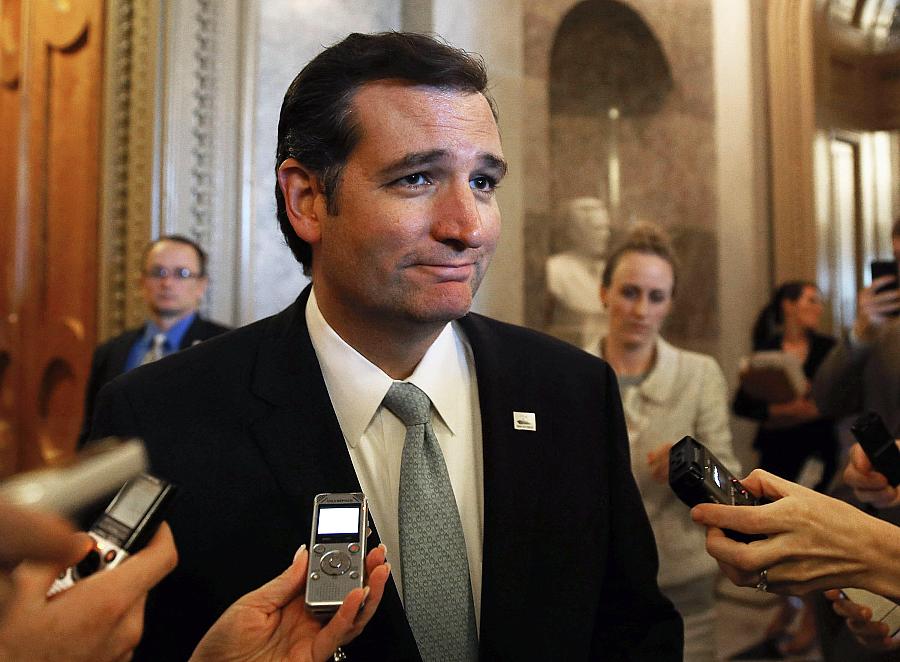
[Photo: Mark Wilson/Getty Images]
