New Medi-Cal rules ease access to hepatitis C drugs
Rebecca Plevin wrote this story while participating in the California Data Fellowship, a program of the Center for Health Journalism at USC's Annenberg School of Journalism.
Other stories in the series include:
A financial case for expanding access to costly hep C drugs
Obesity among Latinos in the San Joaquín Valley: One Family's Response
Samantha Smith checks on 58-year-old patient Paul Shelton. He has severe liver scarring as a result of hepatitis C, but his insurance company has denied his request for treatment at least twice. Susanica Tam for KPCC
California’s revised eligibility rules for hepatitis C drugs appear to be easing Medi-Cal patients’ access to the highly effective medications, according to state data. Yet even with the relaxed guidelines, the vast majority of those on Medi-Cal with hepatitis C still aren't getting the costly drugs, state health officials say.
When the first of the new class of hepatitis C medications were introduced in late 2013, only the sickest people on Medi-Cal could access them. The state Department of Health Care Services had determined that Medi-Cal members needed to have severe liver scarring or cirrhosis to be eligible.
"Our doctor here would say, 'you're almost dead but not dead yet, and that's how we're getting you approved,'" recalls Samuel Gonzalez, who oversees the hepatitis C program at the nonprofit St. John's Well Child and Family Center.
The state revised its hepatitis C treatment policy in July 2015, expanding eligibility to hepatitis C patients with light liver scarring.
The goal of this policy change is "to see as many people who desire treatment, and who qualify for our guidelines, to be treated as possible," says Dr. Julia Logan, chief quality officer in the Office of the Medical Director at the state Department of Health Care Services.
In fact, the policy change has resulted in more people gaining access to the medications, which cure the infection in about 95 percent of patients. The drugs include Sovaldi and Harvoni, made by Gilead, and Olysio, made by Johnson & Johnson. A KPCC analysis of state data finds the rate of people getting denied for the drugs in one Medi-Cal program has dropped from almost two-thirds to just under one-half since the new treatment policy took effect.
"A really large state took a bold move and really reduced the restrictions, and that was a great first step toward sending the message that, 'we understand how important it is to provide treatment access to people living with [hepatitis C],'" says Robert Greenwald, director of Harvard Law School's Center for Health Law and Policy Innovation.
But despite the policy change, very few of the people on Medi-Cal with hepatitis C have received medication.
Of the estimated 250,000 Medi-Cal members with hepatitis C, just 6,460 received hepatitis C drugs between December 31, 2013 and March 31 of this year, according to the Department of Health Care Services.
Treating that relatively small group cost the state nearly $590 million. Sovaldi and Harvoni cost $84,000 and $94,000, respectively, for a 12-week course of treatment.
Some health policy experts say these drugs' high cost led policymakers to erect high barriers to access. But that has not been the case with Medi-Cal, says Department of Health Care Services spokesman Anthony Cava.
"Decisions about which Medi-Cal patients are prescribed the new drugs are based on medical necessity and prior physician authorization" per guidelines set in part by the U.S. Department of Veterans Affairs, "not on cost," he says.
The eligibility policy has also been shaped by input from the American Association for the Study of Liver Diseases, the Infectious Diseases Society of America and other experts, says Cava.
The state's approach to hepatitis C treatment has evolved over the past couple of years as clinical trials and real-world experience confirmed the safety and effectiveness of new drugs, he says.
A two-thirds rejection rate
In an attempt to meet the demand for care, St. John's launched a hepatitis C clinic in 2014. Since then, the clinic's 11 doctors and staff members have seen about 230 patients, says Gonzalez.
About half of them contracted hepatitis C through intravenous drug use, Gonzalez says. Some got it by getting tattoos in prisons, while others are from foreign countries, where they received medications through shared needles, he adds.
Anthony Bellard, 55, of Compton waits to speak to his doctor at St. John's. He recently began taking Harvoni, one of the drugs that treats hepatitis C. Susanica Tam for KPCC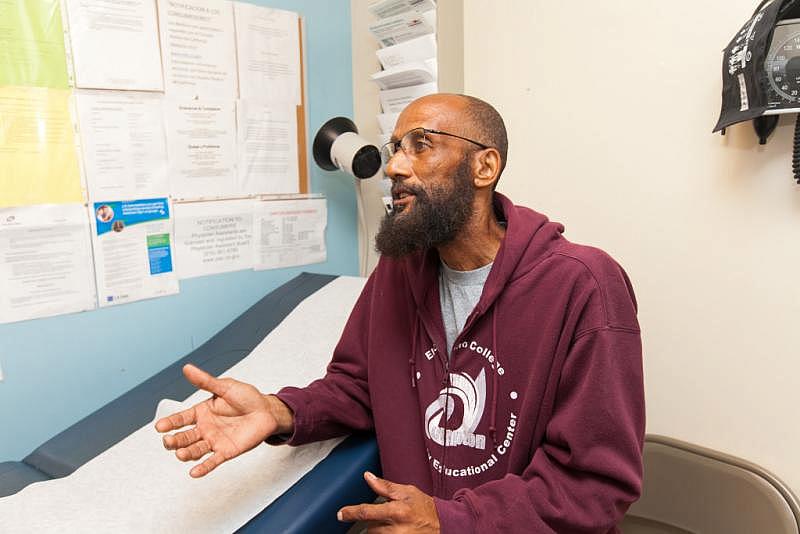
Experts estimate about one-half of the people with chronic hepatitis C don't know they have it. Until recently, that was the case for St. John's patient Anthony Bellard of Compton. He says he used IV drugs in his 20s and got tattoos in his 30s, but he didn't have any symptoms of hepatitis C. He was only diagnosed after undergoing blood work at the clinic about two years ago.
"It wasn't anything that I could notice that would let me know that I had it," Bellard, 55, explains.
Most of the patients in St. John's hepatitis C clinic – and most Medi-Cal patients statewide – are enrolled in Medi-Cal managed care plans. The state could not provide KPCC with prescription authorization data for these plans.
But data from the other type of plan, Medi-Cal fee-for-service, provide evidence of how difficult it was for doctors to obtain these drugs for their patients before the state relaxed the eligibility guidelines.
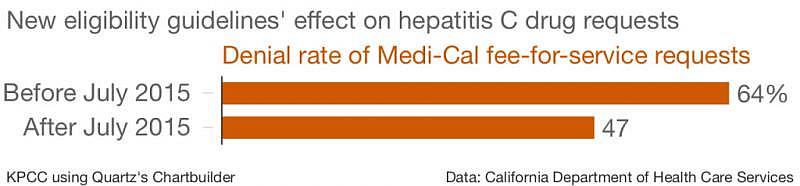
Between January 2014 and June 2015, doctors submitted 1,150 treatment authorization requests for patients on Medi-Cal fee-for-service; the state rejected almost two-thirds of them.
'We were ecstatic'
In July 2015, the state expanded its hepatitis C treatment to include Medi-Cal recipients with light liver scarring. The policy also says people at high risk of spreading the disease – including active injection drug users and women of childbearing age who wish to get pregnant – should get the drug, regardless of their level of liver scarring.
Studies find that between 15-25 percent of hepatitis C patients have light liver scarring, says Dr. Ray Chung, chief of Massachusetts General Hospital's liver center. He estimates that about 50 percent of patients with the disease fall within Medi-Cal's new treatment guidelines.
Gonzalez of St. John's says the change has made it easier – and quicker – to get some patients approved for treatment.
He recalls the case of one woman, whose Medi-Cal managed care plan denied an earlier request for treatment because she had no evidence of liver scarring. Clinic staff felt that, as a woman of childbearing age, she fit the new treatment criteria. So they submitted a new request for hepatitis C drugs, says Gonzalez.
The clinic submitted the request "on a Tuesday and it got approved by Thursday, and we were ecstatic," says Gonzalez.
Other doctors have had similar experiences since the change, says Emalie Huriaux, director of federal and state affairs for Project Inform, which advocates on behalf of HIV and hepatitis C patients.
"One provider, for example, told me, whereas before he felt like he could only get about 20 percent of his patients treated, now he feels like there's 20 percent of his patients he can't get treated," Huriaux says.
State data suggest the revised policy has increased the rate of Medi-Cal fee-for-service patients receiving hepatitis C treatment: In the 18 months before the change last July, the state denied 64 percent of Medi-Cal fee-for-service treatment authorization requests. In the nine months after the change, the denial rate fell to 47 percent.
Utilization 'should be much higher'
But the fact that only a tiny proportion of Medi-Cal members with hepatitis C have received treatment worries advocates like Huriaux.
"Our opinion is that that's very small numbers, given the burden of disease, and utilization should be much higher," she says.
Dr. Samantha Smith treats hepatitis C patients at St. John's Well Child & Family Center. Susanica Tam for KPCC
Sometimes, it's unclear why patients are denied treatment.
St. John's patient Paul Shelton of Compton meets the new eligibility requirements, as he has severe liver scarring from hepatitis C. But his Medi-Cal managed care plan has turned down at least two requests for medication.
"It's not frustrating because I've got my faith," Shelton says. "I'm not really tripping because it doesn't hurt."
But his doctor, Samantha Smith, is very frustrated.
"He doesn't drink, he hasn't used drugs for God knows how long, he's somebody who's taking care of himself and trying to, and he's willing to do 12 weeks of treatment," she says. "Yet we can't get it for him. Yeah, it's a nightmare."
Some patients might be declining medication, says Dr. Logan, with the Department of Health Care Services.
"The hepatitis C treatment, while it's much lower risk and much more efficacious at this point, there are still side effects to the treatment," she says. "People with chronic hepatitis C at lower stages of disease tend to feel well, they're not sick, so they don't feel like they would want to be treated at this point."
Dr. Chung, of Massachusetts General Hospital, says the new drugs are "overwhelmingly well tolerated." He adds that the drug ribavirin, which is sometimes used in combination with hepatitis C treatments, can cause anemia, fatigue or a rash.
"We want these patients to get treated now"
Almost a year after the state expanded its treatment guidelines, several advocates say it's time to open up treatment to all patients with chronic hepatitis C.
Project Inform's Huriaux says this sort of policy would benefit not only those individuals with hepatitis C, but also the broader community, as it would help prevent transmission of the disease. Removing all treatment restrictions would also align Medi-Cal's treatment guidelines with those of the American Association for the Study of Liver Diseases, she says.
Health care providers, case managers, and support staff at St. John's in Los Angeles follow a long and involved protocol to try and obtain medications for their patients with hepatitis C. Susanica Tam for KPCC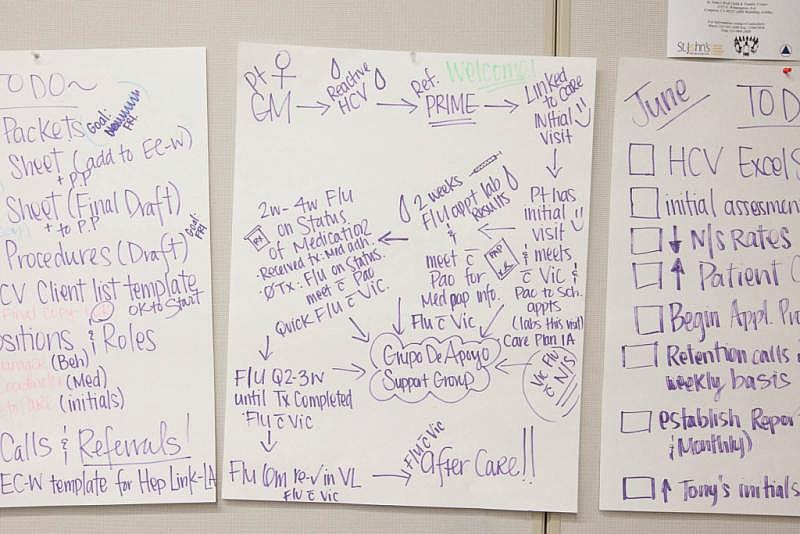
Massachusetts General's Dr. Chung, who helped write the Association's guidelines, says its recommendation that all patients with hepatitis C should be treated has been strengthened by more recent evidence that chronic infection is associated with other complications - including a higher likelihood of developing cardiovascular disease, kidney disease and diabetes - even when patients have limited liver disease.
St. John's, for its part, isn't waiting for Medi-Cal to change its policy. Of the clinic's 230 patients, about 50 have received medication.
"We're submitting prescriptions for pretty much all of our patients that we think can handle the medication and will be adherent," Gonzalez says, while acknowledging that some of those requests are being denied.
Still, "we keep kind of pushing the envelope and keep pressuring insurance companies to treat these patients," he says. "We want these patients to get treated now, because the more people that get treated and cured, the less likely they are to spread it."
Meanwhile, a Department of Health Care Services spokesman says the agency has no plans to further revise its eligibility policy.
[This story was originally published by KPCC.]
Photo Credit Susanica Tam/KPCC.
