Physician aid in dying? Euthanasia? Getting the terminology straight
Last week, just before the California legislature approved a bill to allow physicians to prescribe a lethal dose of medication for terminally ill patients who want to end their lives, MSN reported the news with this headline: “California to Become the Sixth State to Allow Euthanasia.”
Wrong. California is not considering whether to legalize euthanasia of patients. Nor is any other state. Euthanasia of human patients is not legal anywhere in the United States, including the four states that permit physician aid in dying, some of which have laws called death with dignity. (Another error: California would become the fifth state, not the sixth, to permit physician aid in dying. Aid in dying is legal in Oregon, Washington, Vermont, and Montana. It had been legal in New Mexico because of a court ruling, but that was overturned on appeal last month.)
With so many terms that have something to do with physicians and their role in hastening the death of dying patients, it’s understandable that journalists would get confused. But with initiatives to legalize aid in dying around the country and internationally, we need to get clear about what the various terms mean. That’s easier said than done, but here goes.
Euthanasia is “the intentional killing of a patient by a physician, as through the physician’s administration of a lethal dose of medication,” states The Hastings Center Guidelines for Decisions on Life-Sustaining Treatment and Care Near the End of Life. (The terms active euthanasia and passive euthanasia have fallen out of use. Guidelines doesn’t use them, and The Free Dictionary’s medical dictionary says “now all euthanasia is generally understood to be active, and so the more accurate term forgoing life-sustaining treatment is replacing passive euthanasia.”)
Physician aid in dying and physician-assisted suicide (as well as physician-assisted dying, aid in dying and assisted suicide) all mean the same thing. They refer to the prescription by physicians of a lethal dose of medication to patients, upon their request and under certain conditions, for the patients to take if they choose to hasten their death.
For a deeper discussion of the distinction between euthanasia and aid in dying, see Marcia Angell’s review of Atul Gawande’s latest book in The New York Review of Books.
Here’s where things get complicated. For one thing, advocates of aid in dying object to the term physician assisted suicide. Death With Dignity National Center explains its reasoning: “Suicide is generally defined as the act of taking one's own life voluntarily and intentionally – generally as the result of an individual's self-destructive impulse and mental illness and often independent of a terminal illness. Because a terminally ill adult patient who is deemed mentally competent chooses to hasten his or her death through a physician's assistance, ‘physician-assisted dying’ is more accurate than ‘physician-assisted suicide.’”
On the other hand, some who oppose legalized aid in dying prefer the term physician-assisted suicide. My colleague Daniel Callahan, co-founder of The Hastings Center, has called the effort by advocates to replace “physician-assisted suicide” with “physician aid in dying” and its ilk “obfuscation.”
Things get even more complicated when you look at legal practices around the world. In the U.S., for now, physician aid in dying and its synonyms refer only to physicians prescribing lethal medication to terminally ill patients who are mentally competent to request it and who are capable of taking it themselves. However, other countries extend legal aid in dying to some patients who are not terminally ill. Earlier this year, Canada’s Supreme Court unanimously ruled against a law that prohibited “physician-assisted dying” (the term used in the decision). The decision does not seem to be restricted to terminally ill patients. It applies to “a competent adult person who (1) clearly consents to the termination of life and (2) has a grievous and irremediable medical condition (including an illness, disease or disability) that causes enduring suffering that is intolerable to the individual in the circumstances of his or her condition.”
Things get more still more complicated in Europe. Switzerland permits aid in dying and extends that right to foreigners who come to the country to die. Two organizations in Switzerland, Dignitas and Exit, provide physician-assisted suicide (using the term suicide). Euthanasia is legal in the Netherlands and Belgium (subject of a PBS News Hour segment and a recent New Yorker article). The Netherlands permits euthanasia of severely ill newborns, and Belgium allows it for adults who are not terminally ill, as well as for children.
Back to the MSN article – it was a wire story from AFP, a global news agency. International differences in legal practices might have contributed to the confusion of euthanasia and physician aid in dying with regard to the pending California legislation. The name of that legislation introduces yet another term to the mix: “end of life option.”
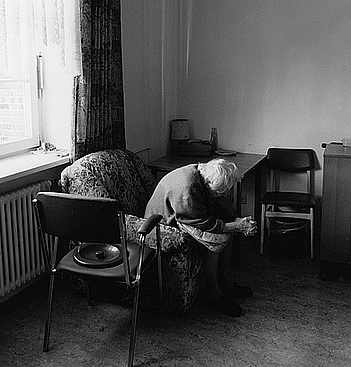
[Photo by Ulrich Joho via Flickr.]

