The myth of telemedicine?
Elizabeth Zach is a staff writer at the Rural Community Assistance Corporation. This article was produced as a project for the USC Center for Health Journalism’s California Health Journalism Fellowship.
Other stories in the series include:
As a young infectious diseases physician in San Francisco in the 1990s, Javeed Siddiqui could easily treat local patients suffering from HIV. As drugs became more effective, he would often simply need to check in with his patients, ask how they were doing both physically and emotionally, and refill prescriptions.
But there were also patients who traveled hours from their homes in northern rural California, taking a day off from work. By the early 2000s, he began wondering what he could do differently, via electronic communications.
Siddiqui, now 50, is today the medical director of the University of California at Davis’ telemedicine program and also of the California Institute for Science and Innovation at the University of California at Berkeley.
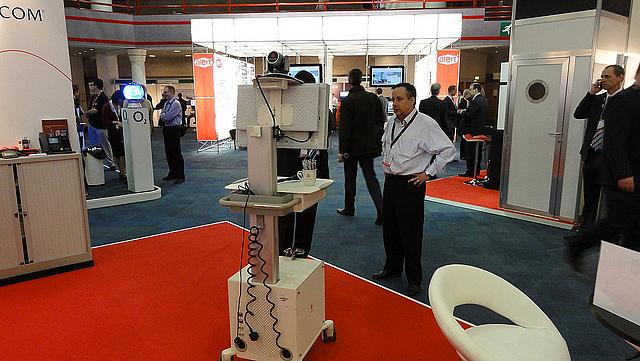
He manages 260 patients across rural California, connecting with them via real-time audio-video conferencing. He liaises with nurses who help with physical examinations and lab work.
“These patients don’t have to travel a ridiculous amount of time to get expert health care,” says Siddiqui, “and they don’t have to take time off of work. It’s been incredibly successful.”
Siddiqui is among many physicians who say telemedicine has the potential to transform health care in some of the world’s hardest-to-reach places, increasing access to care and decreasing its cost per capita. As many rural hospitals nationwide are closing for lack of funding and fewer patients, the prospect and promise of telemedicine is appealing.
“I see economic benefits,” he says. “Laboratory work stays in the community. In terms of productivity, people don’t have to take time off from work to get to doctor appointments. There are only limitations because there is skepticism but I believe that we can bridge that gap. We may not do robotic surgery, but guess what? Having a telemedicine consultation beforehand cuts down on travel time to find out if the surgery is right for this patient, and that’s very good.”
The use of telemedicine is widespread and expanding, said Siddiqui.
“It’s one of the fastest growing segments for healthcare delivery in the nation, not just California, and it’s seen as an important segment of healthcare delivery” he said, noting that in 2015, $20 billion was spent on it nationwide and that that figure will rise to $23.8 billion by the end of this year. Governors, senators, even President Obama, Siddiqui said, have referred to it as a solution in many instances where it’s difficult to deliver healthcare otherwise.
But the technology isn’t a panacea for all that ails rural healthcare today. Some critics point out that rural areas still lack the required internet connectivity to support telemedicine, which is based on high-definition video. Any DSL connection can support telemedicine, Siddiqui said, and in California, the broadband capability more than supplies what is required for telemedicine uses.
Others say telemedicine does nothing to enrich a local economy in the way that a hospital does, providing jobs and a nexus for other community goods, such as schools and property values.
In March, the Journal of Rural Health published a study illustrating that rural hospitals and clinics have significantly slower Internet connections than do their urban counterparts. Between 2010 and 2014, that gap widened, and continues to widen, “a cause for concern,” noted the authors.
“I can’t imagine telemedicine can replace a facility, because you always need a place for people to go,” Marlene Maheu, executive director of San Diego’s TeleMental Institute, says. “You can’t do a video consultation at a McDonald’s. Telemedicine is not designed to treat the full-range of mental illness, such as bipolar disorder or schizophrenia. But it can help with the initial screening.”
Still, as telemedicine gets better and better, it can replace more and more services. The question is whether those benefits can outstrip the decline in services across rural communities.
[This story was originally published by High Country News.]

