Prostate cancer attacks North Carolina black men at startling rate
This series, originally published by The News & Observer, was produced with support from the Dennis A. Hunt Fund for Health Journalism, a program of the USC Annenberg School of Journalism's California Endowment Health Journalism Fellowships.
Other stories in this series include:
Change in screening guidelines incites confusion
Duke expert: New prostate screening guidelines not accurate
UNC expert: Regular care is key to prostate cancer diagnosis
In poor, rural South, reaching black men at risk for prostate cancer is difficult
NC barber has 30 good reasons not to ignore prostate cancer symptoms
North Carolina state official: Funding to fight prostate cancer is tight
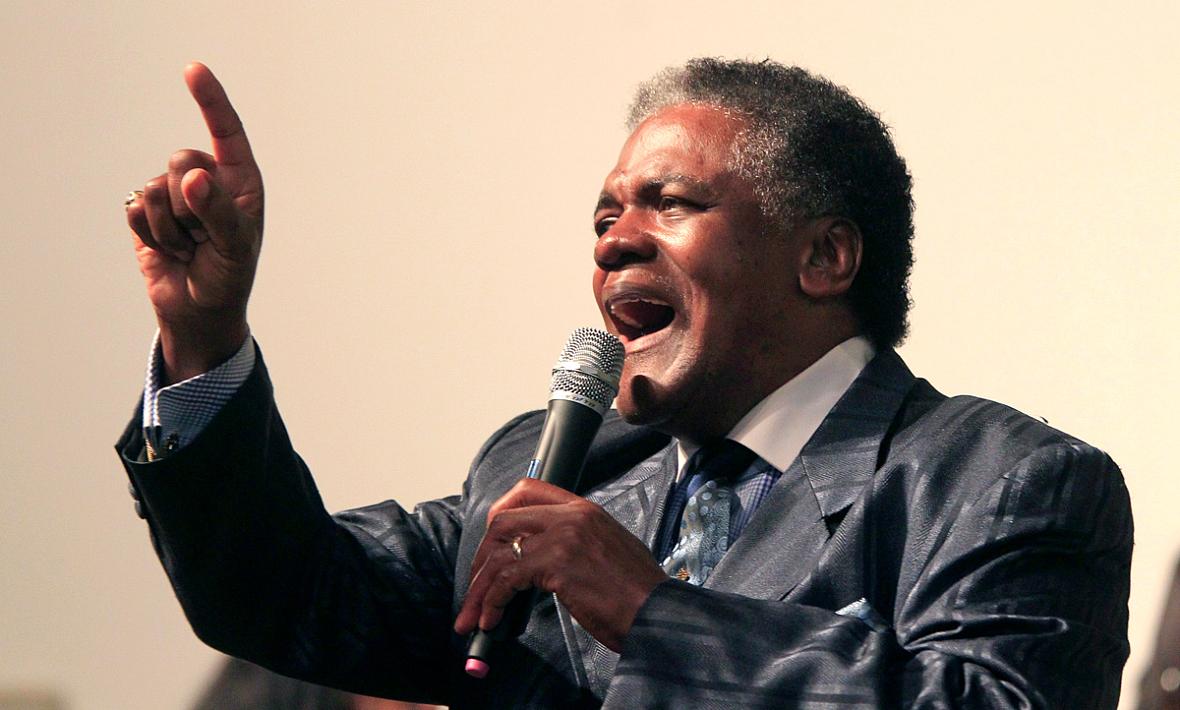
The Rev. Thomas Walker sings during a service at Ebenezer Missionary Baptist Church in Rocky Mount. He was diagnosed with an aggressive form of prostate cancer at age 47 and has become a prostate cancer activist. (Ethan Hyman/News & Observer)
GARYSBURG
In 1997, Halifax Community College math instructor Wendell Perry was diagnosed with an aggressive case of prostate cancer. It was found at what would be an unusually early age for a white man.
But Perry is African-American. So it wasn’t odd that he was facing a threatening form of the disease while still in his mid-50s.
Nor was it strange that he hadn’t been told how common and dangerous prostate cancer was for black men.
Or that he initially didn’t get good care in his mostly rural community, where the only urologist practicing then misdiagnosed the illness, Perry said.
Or that Perry, now 74 and retired, knows more than 10 black men who have been diagnosed with prostate cancer.
The likelihood of black men getting prostate cancer and dying from it represent two of the biggest gaps between the health of black and white men in the United States. The gulf is particularly wide in North Carolina, where the odds of dying from prostate cancer are among the worst in the nation, with African-Americans nearly two times as likely as whites to be diagnosed with it and nearly three times as likely to die from its complications.
For every 100,000 African-American men in North Carolina, 216 per year will develop prostate cancer, and 48 will die of the disease, according to the N.C. Central Cancer Registry.
Perry’s story is startlingly common across a swath of Northeastern and Eastern North Carolina counties, where the African-American population approaches or exceeds 50 percent, and where, for reasons not completely clear, the disease is often even more deadly for black men than the sobering average for black men statewide.
In Northampton County, about 75 miles northeast of Raleigh, black men are nearly four times as likely as whites to succumb to the disease, according to data from UNC-Chapel Hill’s Lineberger Comprehensive Cancer Center.
For black men, prostate cancer is a much more fearsome disease.
“It’s an epidemic,” said the Rev. Thomas L. Walker of Rocky Mount, who was diagnosed with an aggressive form of the cancer at age 47 and has become a prostate cancer activist, spreading the word among black communities about the dangers.
“It has been a tremendous toll, and the nature of the disease perpetuates it and makes it worse because you have to break through that barrier and deal with something that’s really private for many of us,” Walker said.
A book he wrote to get information on prostate cancer to more black men includes detailed information about his own case, including medical records. Walker was diagnosed after developing a standard symptom for middle-aged and elderly men that is often meaningless: struggling to urinate.
After consulting with a doctor in Florida, Walker decided on an aggressive approach to treatment, including radioactive pellets implanted in his prostate. He’s now 66 and says that periodic checkups have shown no issues.
Given the amount of overtreatment that men have received for the disease, it can be hard to tell for sure whether someone who was treated actually was in serious danger. But Walker credits the treatment for saving his life.
“By the grace of God, I believe I made the right decision,” he said.
‘IT WEIGHS ON YOU’
It’s the accepted family story now that if Wendell Perry’s urologist hadn’t himself died of prostate cancer, Perry would never have been properly diagnosed.
Later, his general practitioner didn’t like Perry’s symptoms and sent him to Duke Medicine in Durham for a proper check. Results from the standard, but unreliable, PSA blood test for prostate cancer, which measures the level of a substance put out by the prostate, looked bad.
A doctor then took several biopsies, tiny samples of tissue, from various parts of his prostate.
“They told me I had so many hits, about 11 or 12, that it was really bad.”
Perry decided to have his prostate removed. Now, 17 years after the operation, routine checkups continue to show that he’s healthy, Perry said.
When it hits your family hard, as it has Perry’s, that’s a risk factor that doctors use to evaluate whether you should be screened and, if you are diagnosed, whether your case is likely to be dangerous.
“It weighs on you,” Perry said, “but what can you do except move on and try to keep your life together?”
Many of the hardest-hit counties around the state are rural and impoverished, and some have only a handful of doctors, if that. Outreach efforts to get accurate information about the disease to black men have sometimes been as rare as doctors’ offices where it can be diagnosed and treated and as scarce as the money to pay for health insurance.
About 300 African-American men die from prostate cancer in North Carolina every year. If the mortality rate were brought down to the same level as for white men, nearly 200 of them could be saved.
But the barriers to that are numerous, one long string of daunting bottlenecks. Some may be biological and harder to discern, though researchers are trying. Some are cultural, some socioeconomic, some tied to lack of insurance, some to lack of access to medical care. Those things can mean the cancer is found later, when treatment is less likely to succeed.
“If you’re an African-American male, you’re probably the least likely person to be in the preventive, health-seeking mode for any issue, and that’s been time-tested,” said Allen Smart, vice president for programs at the Kate B. Reynolds Charitable Trust, based in Winston-Salem. The organization funds projects to improve the health of low-income North Carolinians.
“Males are less likely than women, and African-American males are less likely than white males, to be health care seekers, and then when you include the access barriers and the levels of uninsured and underinsured, then you’re painting a picture of a public health crisis that people have, I think, come to think of as the norm,” he said. “And that’s really unfortunate, because it’s incredibly treatable, and in many cases a good regimen of care will get you back on your feet.”
A QUESTION OF SCREENING
The prostate is a walnut-sized gland that secretes fluid that nourishes and protects sperm. That fluid is expelled with sperm as semen during ejaculation.
In some ways, prostate cancer behaves oddly. It’s the most common non-skin cancer among U.S. men. But nearly two-thirds of all cases are diagnosed among men older than 65, and it usually grows so slowly that those who have it die of something else. More than 200,000 Americans are diagnosed with it each year, or about 138 per 100,000 men, and about 29,000 die from it, about 21.5 per 100,000.
In African-American men, though, it tends to appear not only more often but at an earlier age. It’s also more likely to be dangerous and fast-moving. And catching it early recently has become trickier: The usefulness of the standard blood test for prostate cancer has come under serious question. The ensuing debate over its merits has driven some away from testing.
It’s hard to say which of the many barriers is the first on the long road to getting a high-quality regimen of care. But near the top of that list is availability and accuracy of the information that black men get about prostate cancer screening.
Screening for the disease is one of the most controversial topics in medicine, mainly because of a recommendation announced in 2011 by the U.S. Preventive Services Task Force, an independent group of health care professionals that develops disease prevention policies for the federal government.
The task force recommended that healthy men of all races stop getting screened for prostate cancer with the PSA test, which measures the level of a substance released by the prostate gland into the blood. The panel concluded that, while screening with PSA probably saves some lives, it leads to unnecessary surgeries and other treatments that harm patients who otherwise might survive the cancer with little or no problem.
The recommendation led other groups, such as the American Cancer Society, to modify their own guidelines, made it harder for federally funded programs to get money to pay for screening and led some community groups to stop offering free screening events.
MISTRUST OF MEDICAL INSTITUTIONS
But the new guidelines, it turned out, were developed without significant data on the effects of screening black men.
Dr. Durado Brooks, director of prostate and colorectal cancers for the American Cancer Society, has spent much of his career trying to enhance prevention in primary care and to improve care for medically underserved populations.
“The message that men get now is kind of confusing to say the least,” Brooks said. “The task force simply said men shouldn’t be screened, but if you dig down in their recommendations, they note that they don’t have enough data on black men to say anything about how screening affects them.”
Black men are more likely to be uninsured or underinsured than their white counterparts and less inclined to have regular checkups. Yet they are disproportionately affected by prostate cancer and other diseases, including sickle cell anemia and diabetes.
Research, including studies in North Carolina, has shown that black men tend to mistrust the medical establishment – in part a legacy of a notorious, four-decade study performed on black men at the Tuskegee Institute in Alabama. Federal researchers there studied hundreds of black men with syphilis from 1932 to 1972 and, even after a treatment was found, withheld it and watched to see what the disease would do to them.
And that’s one reason the task force recommendations didn’t have enough data to apply to black men: They are less likely to sign up for research studies.
A debate over the screening recommendations continues to rage in the medical community, with some thinking the task force guidelines make sense for all, some believing that they are more applicable to white men and others thinking that they’re completely wrong.
Experts on prostate cancer think that the confusion raised by that debate and the changes to the screening recommendations have made it even more difficult to persuade African-American men to see doctors or trust whatever they hear about prostate cancer.
“The way it was portrayed in some media outlets, words were being spoken like ‘Prostate cancer screening is killing men, not saving men,’” said Steven Patierno, deputy director of the Duke Cancer Institute, who does research on the genetics of the disease in black men. “Now, that’s a wonderfully controversial, eye-opening message for a reporter to latch onto and get it into a newspaper or on the nightly news.
“It fed into every innate fear that you could possibility find in the African-American community, and they played on that over and over and over again. And it did an incredible amount of damage.”
Patierno – like many other experts who are unhappy about the task force guidelines – recommends a careful, personalized approach. The idea is for health care professionals to educate men about their risk and about screening so they can make an informed decision.
There are essentially two parts to the racial gulf in the death rates for prostate cancer. Some can be fixed, in theory at least: typical underpinnings of public health problems, such as the need for better nutrition, exercise and access to high-quality health care.
But even if those were fixed, many researchers believe, another cause would remain: There may be biological differences in the tumors. So far, researchers have not been able to unlock those differences and develop targeted treatments as they have for, say, certain breast cancers.
Some of the studies have included people in the northeast counties, including Perry.
It’s frustrating, he said, that researchers have visited the area several times without seeming to come up with anything that helps.
“I’ve answered questions and filled out forms, and nothing has changed, nothing,” he said. “People spend money after money, and there’s study after study, and we’re in the same position.”
