Will children’s uninsured rate double if Obamacare is repealed?
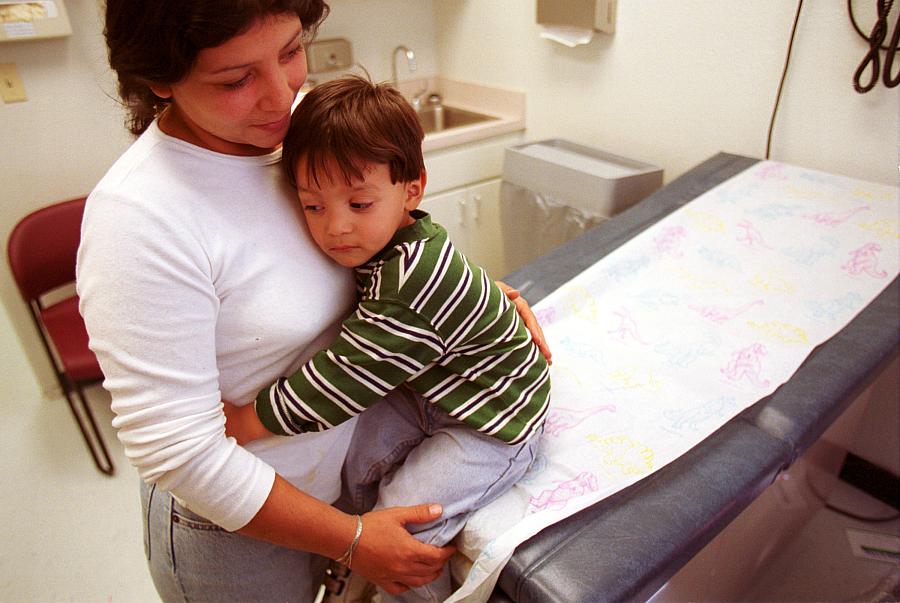
Photo: Joe Raedle/Getty Images
For the past two decades, the share of children lacking health insurance has steadily declined.
In 1997, the same year Congress passed the Children’s Health Insurance Program (CHIP), about 14 percent of children under the age of 18 were uninsured. By 2015, that figure had dropped to 4.8 percent, a historic low. The gains have been especially sharp since 2013, as the Affordable Care Act took effect.
That long trend of steady gains in the rate of children’s coverage could be reversed, however, under the widely expected repeal of the Affordable Care Act and changes to how Medicaid is funded, according to recent projections.
The Urban Institute published a widely reported brief earlier this month that looked at what a partial repeal of the Affordable Care Act — including a reversal of the Medicaid expansion — would mean for health coverage in the coming years. Children make up a small percentage of the roughly 30 million people Urban says would become uninsured by 2019, but the numbers still represent a dramatic uptick: The share of uninsured children would rise to 9.6 percent by 2019, according to the brief.
Only 6 percent of children in 2015 received insurance in the non-group market, so relatively few children would be directly affected by the elimination of Obamacare subsidies or the market’s outright collapse, as some expect will happen if the requirement for coverage of pre-existing conditions doesn’t continue to be coupled with the mandate to seek insurance coverage and subsidies.
But Medicaid and the Children’s Health Insurance Program covered nearly 40 percent of U.S. children in 2015, so the rollback of the ACA’s Medicaid expansion and changes to how those programs are funded — Trump has called for block granting Medicaid — could have major effects on kids. And CHIP will face a major test in the coming year since funding for the program expires on Sept. 30, 2017. Republicans proposed changes to the program last year that would’ve allowed states to restrict eligibility and increase the waiting period for kids seeking to enroll after losing coverage from a parent’s plan.
“The Affordable Care Act, which maintained and enhanced existing Medicaid and CHIP coverage for children, led to widespread declines in the number and rate of uninsured children from 2013 to 2015,” concluded an October report from Georgetown University’s Center for Children and Families.
According to Urban’s forecast, “State spending on Medicaid and CHIP would fall by $76 billion between 2019 and 2028.”
The Affordable Care Act has led to further gains in children’s coverage in several ways. These include essentially administrative changes, such as making enrollment simpler (“no wrong door”); giving families more time between renewals of coverage; and making it faster and easier to do so. (Louisiana, for example, uses data from its food stamp program to determine Medicaid eligibility and “fast track” enrollment.) Obamacare also curtailed states’ ability to impose onerous waiting periods for kids trying to enroll in CHIP.
The legislation also stopped states from stiffening their Medicaid/CHIP eligibility rules for a decade, as the Kaiser Family Foundation explains:
The ACA protects the gains already achieved in children’s coverage by requiring states to maintain eligibility thresholds for children that are at least equal to those they had in place at the time the law was enacted through September 30, 2019.
It seems unlikely that any Republican replacement would extend such a federal restriction on states. In a follow-up Urban analysis, researchers estimate that if all states were to lower their eligibility standards to the federal minimum, an additional 8.9 children would lose coverage.
That’s very worrying to children’s policy experts such as Georgetown’s Joan Alker, who recently wrote:
States will likely have more flexibility to limit children’s coverage under most conceivable scenarios in 2019, and they may well have less federal money to pay for it, which may be an incentive to do so.
But one of the biggest ways Obamacare led to more insured kids isn’t through anything codified into law. Instead, it’s something called the “welcome mat effect,” kissing cousin to the “woodwork effect.”
As studies have shown, when parents start looking into their own health coverage options, they’re much more likely to discover their kid is eligible for Medicaid or CHIP and enroll them. Conversely, if a parent no longer qualifies for Medicaid or decides to forgo insurance in a world where it’s no longer mandated, then children in that family are less likely to find coverage as well.
We’ll no doubt learn more in the weeks and months to come about what will be in a Republican plan to replace Obamacare. But based on the GOP’s last reconciliation bill, which Obama vetoed in January 2016, the downward trend on rates of uninsured children may have nowhere to go but up, for the first time in decades.
**
Related posts
Election result could have major implications for children’s coverage

