The Name Game and Chronic Fatigue Syndrome: DSM-5 Revisions Should Be Openly Debated
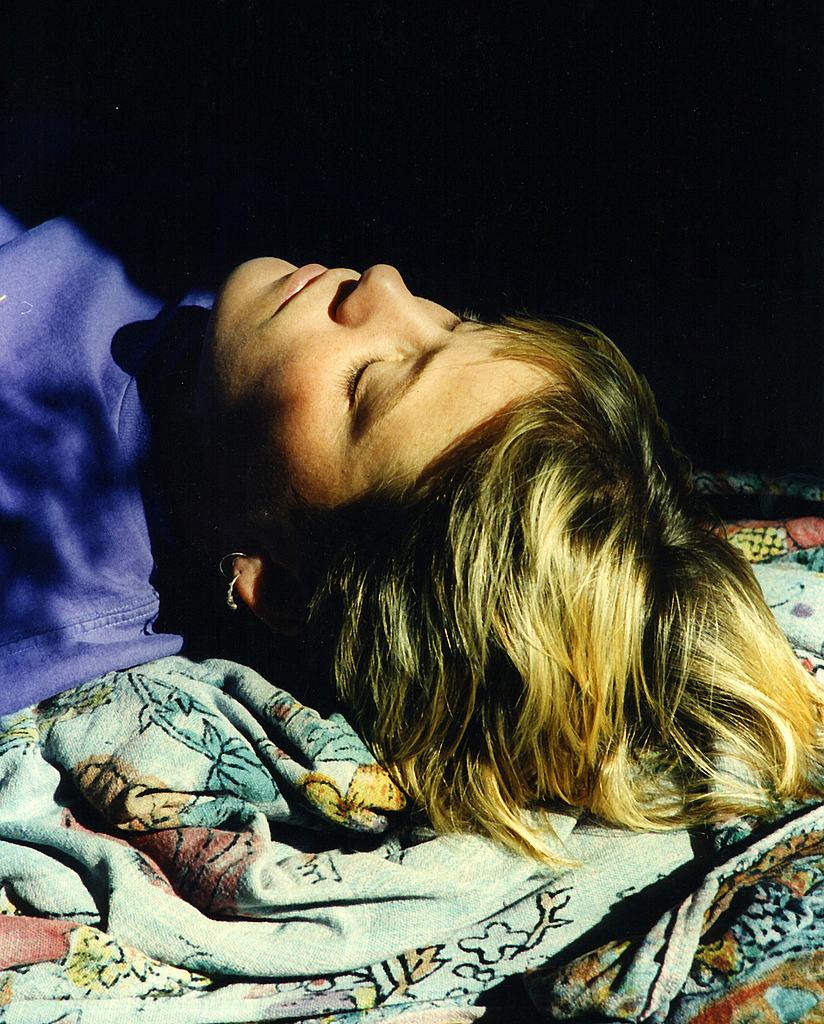
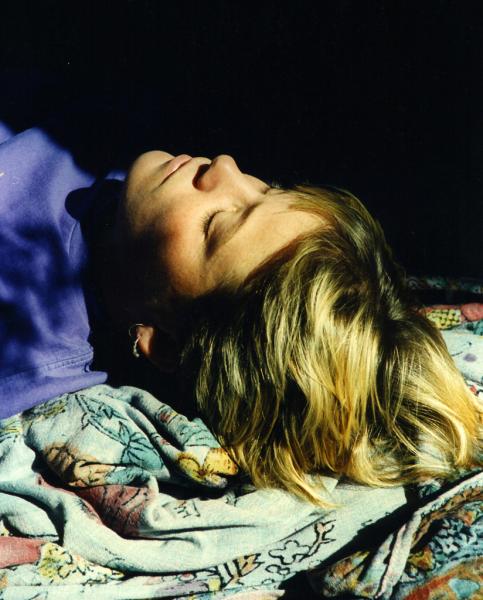 Mary Schweitzer writes a blog called Slightly Alive that takes its name from a bit of dialogue in The Princess Bride. With a droll wit and an acute eye for medical detail, Schweitzer tries to give voice to the millions of people who suffer from difficult to diagnose health conditions, such as chronic fatigue syndrome (CFS). She was an associate professor of history at Villanova University before a prolonged illness forced her to quit in 1994. As she described to me:
Mary Schweitzer writes a blog called Slightly Alive that takes its name from a bit of dialogue in The Princess Bride. With a droll wit and an acute eye for medical detail, Schweitzer tries to give voice to the millions of people who suffer from difficult to diagnose health conditions, such as chronic fatigue syndrome (CFS). She was an associate professor of history at Villanova University before a prolonged illness forced her to quit in 1994. As she described to me:
I have been diagnosed with CFS (chronic fatigue syndrome) and re-diagnosed with myalgic encephalomyelitis (ME). I have immune defects and several sub-acute, active viruses, plus three strains of coxsackie B. That goes along with significant cognitive and neurological impairment. At one point I could not brush my own teeth and spent most of my time lying in a dark room listening to favorite movies.
Schweitzer sent me a note after I wrote about Suzy Chapman of the blog formerly known as DSM-5 and ICD-11 Watch. This debate about the revisions to the DSM-5 is so contentious, and I am such a novice when it comes to mental health, that I don't have a clear idea of the best way for the American Psychiatric Association to revise its manual and incorporate critiques from Schweitzer and others. I found Schweitzer's ideas so compelling that I asked her to write a guest post. There may be good reason to alter the framing around chronic fatigue syndrome and other conditions, but if critics are going to be silenced, or even just ignored, it could be hard for people to have faith in the eventual outcome. Schweitzer's post is below:
The very thought that the American Psychiatric Association is attempting to protect a "brand" by going after DSM-5 Watch is appalling.
Last time I looked, the APA portrayed itself and the discipline of psychiatry as a scholarly activity. There can be no scholarship without criticism, and there can be no criticism without reference to that which is being criticized.
The deep secrecy which has enveloped the fifth revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is itself a violation of professional ethics. The process around revising and updating the DSM should be an open process, as the content affects so many people's lives.
What could have possessed the APA to use its weight instead to censor a website offering information and intelligent criticism?
There is a growing concern that the discipline of psychiatry has been grabbing more and more territory for itself. When presented with a complex set of symptoms, psychiatry could answer honestly, "we just don't know." Instead, it adds more and more diagnoses to the list of "mental disorders."
Does the psychiatric profession really want to play that role? "I don't know what's wrong with you. It must be psychiatric." Could some of these problems being labeled as "mental" have a different cause?
With the last revision of the DSM, DSM-4, there was a lot of criticism (and jokes) about suspect diagnoses. I thought the discipline (in the United States at least) had done a good job in the last two decades of redeeming itself.
But lately, suspect diagnoses from overseas have been creeping in. When Munchausen Syndrome by Proxy was abandoned as a serious diagnosis in the U.S., it was all too quickly changed to "factitious Illness by proxy."
There is now a group of psychiatrists who are pushing "factitious illness" and the new diagnosis of CSSD - Complex Somatic Syndrome Disorder. CSSD fits the definition of CFS created by Dr. Keiji Fukuda and colleagues in 1994 uncomfortably well. A key aspect of both definitions is that in order to have this disorder, you have to have more than four symptoms.
Name changes are nothing new to suffers of ME/CFS. The disease was called atypical polio for 20 years. Then in the 1950s, it was renamed myalgic encephalomyelitis (ME) and as such has been coded under neurology in WHO's ICD's since 1969. ME also has been a diagnosis used in the United Kingdom and British Commonwealth nations for 55 years.
Initially, the U.S. chose a different name, epidemic neuromyesthenia, but that term fell into disuse by the 1970s. When clusters of cases began to occur in the mid-1980s, U.S. doctors had no name for what they were looking at. Had the outbreaks occurred in Surray, England, however, the patients would have been diagnosed with M.E. In the U.S., the term CFS became dominant.
It may seem trivial to those who don't suffer from ME/CFS, but names do matter. And this name change is particularly important. If this faction of psychiatrists is able to create a CSSD definition in both DSM-5 and ICD-11, they will have succeeded in diverting attention away from a root medical cause for conditions such as ME/CFS and in putting those conditions and other squarely in the realm of psychiatry. This has implications not only for helping ill people get well but also for how insurance companies are going to assess the associated costs. For a change like this to be made, the public should be made very aware of the evidence and the process of evaluating the evidence.
I was a very productive researcher before becoming ill, and my career was on the rise before it was cut short at the age of 44. I am very serious about the absence of scholarly ethics in this entire process. I take scholarship seriously. It was my life. My father was a professor. My husband is a professor. It's kind of the family business.
Who gets hurt by the type of silliness now happening with APA's threats against Suzy Chapman? Aside from the hit that psychiatry takes to its own integrity, the weak in society are the most vulnerable: the poor, children, and in the case of psychiatry, women. Heavily gender-biased diagnoses are all too common in psychiatry. Factitious illness by proxy, for example, is almost always blamed on Mom.
A medical manual should be a compendium of evidence from peer-reviewed literature and established best practices. It is no place to try out new concepts.
If psychiatry wishes to retain its standing as a scholarly field based on scientific research, the hijacking of diagnoses by a closed cabal must not be permitted. Period.
Related Posts:
Slap: American Psychiatric Association Targets One DSM5 Critic, Ignores Others
Slap: American Psychiatric Association Pressures Brit DSM5 Blogger Suzy Chapman
Autism Diagnosis: About That DSM 5 Story
Changing the Definition of Autism: A National Debate Heats Up
Photo credit: anoldent via Flickr

