California becomes first state to offer health insurance to all eligible undocumented adults
The story was originally published by the Calo News with support from our 2023 California Health Equity Fellowship.

California became the first state to offer full health insurance to undocumented immigrants.
Getty Images
Veronica Granados, a 49-year-old immigrant originally from Guanajuato, Mexico will be able to receive Medi-Cal for the first time.
On Monday, California became the first state in the nation to offer health insurance to all eligible undocumented immigrants. Beginning January 1, immigrants of all ages will be eligible for the state’s health insurance program for low-income people, known as Medi-Cal.
Throughout the years, Granados has developed a list of chronic and degenerative diseases.
Full-scope Medi-Cal will allow immigrants like Granados, living in the Golden State to seek free dental, vision care, specialist appointments, mental health care, substance use disorder services, prescription drugs and medical supplies, and in-home care if they meet all Medi-Cal eligibility rules, including income limits.
Immigrants ages 26-49 are the last group to join the ongoing Medi-Cal program expansion, which is part of the “Healthy California for All” initiative, which took effect in 2015. Nine years ago, former Gov. Jerry Brown signed a law making undocumented children (1-18 years old) eligible for state insurance.
What followed was the Young Adult Expansion, which was signed into law in 2019 and provided full-scope Medi-Cal to young adults 19 through 25. In 2023, the Older Adult Expansion, which provided full-scope Medi-Cal to adults 50 or older, was signed into law.
Adults can apply to Medi-Cal online, in person through Medi-Cal enrollment centers and thousands of certified enrollers and over the phone. For California immigrants to qualify for Medi-Cal, adults must submit proof of income that proves their household earns less than 138% of the federal poverty level (FPL), along with additional details like age, marital status, tax information and identification.

Granados lives in South LA and has taken on gardening to improve her holistic health.
Photo provided by Veronica Granados
Granados’ first health issue began as a kid in Mexico when she was diagnosed with epilepsy, a neurological condition involving the brain that makes people more susceptible to having recurrent, unprovoked seizures. “We didn’t grow up with much, but my mom always cared for me, even when she didn’t know what exactly was wrong," she said.
Granados grew up in a small town in Guanajuato, Mexico, where her parents and grandparents lived off the land as farmers. “My parents taught me to value everything—every meal, every day that we get to wake up and although my health has not been the best in the last few years, I remain grateful,” she said.
She immigrated to the United States in 1998 and shortly after she was diagnosed with Sjögren's syndrome, a chronic autoimmune disorder caused when the immune system attacks the glands, which causes the eyes, mouth, and other parts of the body to retain moisture. Granados said that for her, it causes her mouth to feel very dry, a symptom that has required her to visit the dentist more frequently than most people.
She began noticing the ways that not having insurance played a key role in the type of care she would receive. “When I first started going to the clinic because of my severe migraines, they would prescribe me Tylenol and other people would be offered medical tests and examinations to find the exact cause of the headaches,” Granados said.
But the chronic disease that first sent Granados to the hospital for days was fibromyalgia, a chronic disorder that causes pain and tenderness throughout the body, as well as fatigue and trouble sleeping. “It’s the type of pain that you cannot control or get rid of; it's very scary,” Granados said.
She was first diagnosed with fibromyalgia about 5 years ago when the pain was so severe that her husband decided to take her to the emergency room and ask for her to be admitted to the hospital, a decision that would leave them financially struggling. “The doctors explained that they did not know what caused it, but that it explained my heightened sensitivity to pain in my back. I could not walk,” she said. “We spent all of our savings on being in the hospital and seeing a specialist. “
After years of experiencing severe symptoms of fibromyalgia, Granados' feet and entire body are not as strong. She uses a cane to support herself; she cannot walk or stand for long periods or carry heavy equipment; and she gets very cold easily, all of which affect her daily life, her job and her ability to perform regular tasks.
For those like Granados who already have an active restricted or emergency Medi-Cal insurance plan, they will not need to submit their application or apply again. “Those people will be automatically switched over to full-scope coverage beginning January 1st, 2024,” Jose Torres Casillas, Policy and Legislative Advocate at Health Access California, said.
He said that Health Access California had been actively recommending community members and other community organizations to enroll qualified immigrants into emergency-scope Medi-Cal before the beginning of the year, so the transition would be seamless.
Medi-Cal will cover an additional 700,000 Californians
In the United States, one in five (20%) immigrant adults reported having problems when it came to paying for health care in the past year and 22% said they skipped or postponed care in the past year because of their inability to pay, according to a 2023 survey by the LA Times and the Kaiser Family Foundation (KFF).
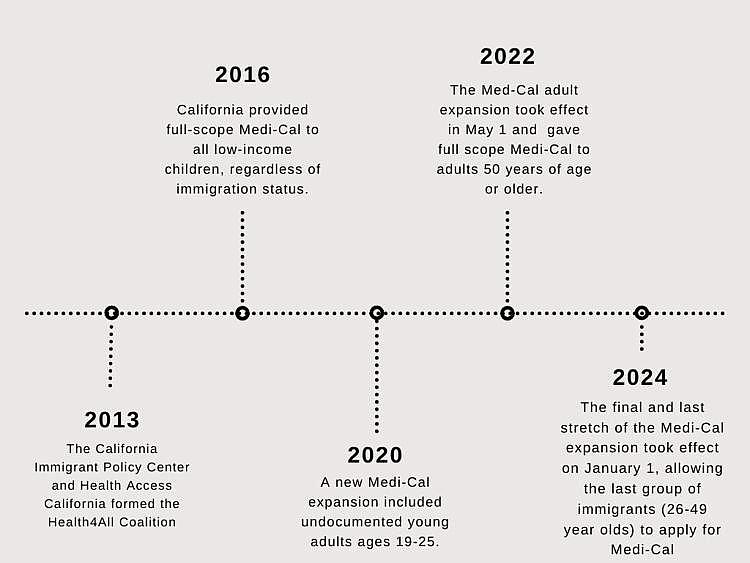
Timeline of the Medi-Cal expansions that took effect throughout the year.
Graph by Brenda Verano
Previously, many undocumented immigrants like Granados only qualified for restricted Medi-Cal, which allowed immigrants to receive emergency and pregnancy-related services as long as they met eligibility criteria like economic requirements and had proof of California residency in 2014.
Medi-Cal provides services to over 13 million Californians (or one in three who rely on the program for health coverage). Granados is excited to begin receiving full-scope comprehensive health insurance, which will help her see a doctor for her chronic pain regularly and can ultimately cover at-home assistance and care, all while not having to worry about the cost.
The California Department of Health Care Services (DHCS), which administers Medi-Cal, estimates that with this new expansion, an additional 700,000 Californians will now be enrolled, but Torres Casillas, said the number of new enrollees will most likely be a lot greater.
“When the 50-year adult expansion was approved, our original estimates were that about 250, 000 people were going to enroll. We're now over 300,000 people over the age of 50 who have enrolled," he said. “We're expecting a similar situation with that of the 26 to 49, where we are currently estimating 700,000 people will be eligible, but we're expecting a lot more people to enroll.”
#Health4All campaign
Torres Casillas has become a policy expert at Health Access California, which serves as the co-chair, along with the California Immigrant Policy Center, of the #Health4All campaign, which has driven the efforts of all the Medi-Cal expansions throughout the years. The Health4All campaign began in 2013 when immigrant rights activists, healthcare advocates, and community members came together to call for expanding health care to all immigrants living in California.
“We're ensuring that we, along with other organizations advocating for immigrants, are at the decision-making table to be able to speak on and address a lot of the issues that exist within the implementation of these Medi-Cal expansions,“ he said. “We want to make sure that the state is able to use a lot of the lessons learned from our prior expansions and apply those to the new expansions.”
The January 1 expansion will cost the California Health and Human Services Agency $835.6 million in funding between 2023 and 2024 and $2.6 billion annually, but Torres Casillas believes these costs are worth the well-being of immigrants. “We need to invest in our immigrant community's well being, and this is a huge step for them to feel supported and part of our country’s health care system,” he said.
Existing flaws in Medi-Cal’s Application Process
However, according to David Kane, senior attorney at Westen Center for Law and Poverty, an organization that has worked closely with DHCS to ensure the implementation of the expansion, the Medi-Cal applications and the application process still have flaws.
“We convene meetings with partners, advocates, stakeholders and the Department of Healthcare Services to make sure that they are implementing this in a way that will meet the needs of the community,“ he said.
For Kane, aside from complaints of Medi-Cal applications that take long to process, adults not being able to reach the county by phone or not being able to get help in their language, one of the biggest flaws in the Medi-Cal application is the section that asks people for their social security number. Although skiing for an SSN is something that is a federal requirement, it is not something undocumented immigrants do not have.
“That's something that should have been fixed a long time ago. We do not want people to feel discouraged when they see this in the application. We need to find a way to let people know they can still get full-scope care even if they don't have a social security number,” Kane said.
Enrollment Barriers
The KFF also found that among immigrants who are eligible for health coverage, many remain uninsured because of a range of enrollment barriers, including fear, confusion about eligibility policies, difficulty navigating the enrollment process, and language and literacy challenges.
For Maria Hernandez, 23, who has had Medi-Cal insurance for over 5 years and speaks fluent English, navigating Medi-Cal is still a challenge. She was born in Puebla, Mexico and immigrated to the U.S. when she was only six months old. “We never really got any assistance or help [from the government] before. My mom was scared of telling people she was an immigrant,” she said.
Hernandez got severely ill during the COVID-19 pandemic, and being able to go to the hospital or clinic to get the appropriate care made her appreciate having health insurance. “It has helped me a lot, just by the fact that I was able to be seen,” she said.
As a former personal translator for her mom, she realized the way language plays a part in health coverage. “I did not live too far from a hospital and being able to go without having to think of the cost or if [doctors] were going to speak English is something I did not have to worry about, but many did,” Hernandez said.
Andrew Kazakes, senior attorney at the Legal Aid Foundation of Los Angeles (LAFLA), has provided free, high-quality legal services to those seeking government benefits, including Medi-Cal. “Part of our work at LAFLA is that we hold clinics set up in L.A. County hospitals, where social workers will refer patients to our clinic if they have any legal issues that might have prevented them from getting approved for the services they need, such as Medi-Cal.”
Although federal funding restrictions limit the assistance LAFLA can provide to undocumented immigrants, with exceptions that depend on individual circumstances, the organization aims to assist uncovered Californians who are eligible for their services, and to provide high-quality referrals to those who they cannot serve directly.

Andrew Kazakes with Dr. Dennis Wong at Rancho Los Amigos National Rehabilitation Center.
Photo provided by Kazakes
During his time hosting legal aid clinics at Rancho Los Amigos National Rehabilitation Center, located in Downey, he worked with many patients who were unfamiliar with the healthcare system of California and who wrestled with navigating Medi-Cal and the application process.
“There was definitely a high volume of undocumented folks who got referred our way. It's really confusing for a lot of people to navigate these different administrative systems and it's not their fault,” Kazakes said. “The system itself is really confusing. Doctors will struggle, social workers will struggle, and even attorneys will have to struggle to figure out, based on somebody's status, what sort of assistance they can get.”
According to Kazakes, because a hospital does not turn away anyone who does not have health insurance or cannot pay, the patient would often obtain presumptive eligibility for Medi-Cal.
“If you have someone who's showing up from a car crash, the hospital doesn't want to pause care; therefore, the patient would get presumptive eligibility, but after the patient receives the care needed, like, for example, a surgery, they are left to transition off Medi-Cal unless they can establish their eligibility,” he said. “It creates this situation where people have already been through trauma, and now they're put in this position of not knowing if the care is going to be there to help them with the aftermath of the accident and fully recover beyond the immediate emergency.”
Kane and Torres Cassillas believe that the hardest part, other than implementing the Medical 26-49 Adult Expansion, will be modifying the Medi-Cal health system to make immigrants feel welcomed and seen. "It's not as simple as saying: 'OK, immigration status doesn't matter anymore.' That's what the law says. It's super clear; it's super simple, but the Department of Health Care Services has historically excluded this group of people. The State Department of Health Care Services needs to break down the systemic barriers that they have had in the design of their program,” Kane said.
Supporting New Medi-Cal Patients
Katie Rodriguez, vice president of Policy and Government Relations at the California Association of Public Hospitals and Health Systems (CAPH), said their members are excited to welcome new full-scope Medi-Cal patients and wants them to feel supported in the clinics and hospitals where they will be seeking care.
According to Rodriguez, 21 public hospitals and their clinics in the state, such as Los Angeles General Medical Center and UCLA Medical Center, already see many of the patients that have recently become eligible for full-scope Medi-Cal. “The majority of our patient population at our public hospitals and healthcare systems are already Medi-Cal or Medicare patients or uninsured,“ she said. “We are very proud of this.”
Rodriguez said public hospitals and clinics do not turn anyone away because of a lack of insurance and are excited to continue to foster the patient-relationship practices that make new full-scope MediCal-eligible patients feel included and seen. “Public hospitals and their clinics regularly communicate with any new and existing patients that come in and make sure that they're aware of all coverage options, in case they're eligible for full-scope Medi-Cal or other services as well,” Rodriguez said.
Rodriguez said she is aware of how filling out new applications can be overwhelming and difficult for people who are doing this for the first time. One of the things that the public hospitals and their clinics have done to ease some of these nerves and assist new Medi-Cal patients is to have people solely designated to help fill out applications and determine eligibility. “Many of our hospitals and clinics have what we call enrollment counselors onsite that help individuals apply,” she said. “Most importantly, the enrollment counselors, tell them what Medi-Cal is, the documentation they need, and what the application looks like. Whenever possible, they go through it with them in the language they feel most comfortable with,” she said.
Public Charge
In August 2019, former president Donald Trump announced a public charge policy that, at that time, could result in the rejection of many immigrants applying for an immigrant visa (e.g. green card) if they had previously accessed or were deemed likely to rely on certain forms of public assistance, such as Medi-Cal. The unenrollment and decreased participation in government assistance programs contributed to more uninsured individuals and negatively affected the health and financial stability of families.
Even as the former public charge rule is no longer in effect and the government has stopped following the Trump-era rule on March 9, 2021, the narrative continues, and according to Torres Casillas, immigrants continue to be afraid of taking advantage of programs like Medi-Cal.
“That rule is no longer in effect, but we're still dealing with the remnants in the sense that people may not know that it's no longer in effect. And if that information spreads, then other people are confused and therefore hesitant to apply to Medi-Cal,” he said.

Andrew Kazakes with his colleague and a patient at Rancho Los Amigos National Rehabilitation Center.
Photo provided by Kazakes
Kane said that the Western Center for Law and Poverty and other immigrant rights advocates, including the Health4All Coalition, continue to push DHCS to educate people on the way public charge is not something they should worry about.
“For some time, DHCS would not want to say anything about public charge because they said it was like giving immigration legal advice, but it's not if you are just educating people,” Kane said. “We've been pushing DHCS to tell people very basic things about public charge, and we've made some great progress.”
Today, DHCS’s website contains basic information on public charge and assures people that the U.S. Department of Homeland Security (DHS) and U.S. Citizenship and Immigration Services (USCIS) do not consider health, food, and housing services as part of the public charge determination. “DHS strongly encourages these populations to access any and all services and benefits available to them without fear of a future negative impact,” states the DHCS website.
For Granados, a flawed Medi-Cal program is better than not having any insurance at all. "I'm still grateful and even if flawed, I’m excited to be able to have Medi-Cal,” she said.
Torres Casillas believes outreach, marketing and informing community members of their eligibility are the most crucial steps after January 1. “People may not know that they're eligible; people may not know that coverage was expanded, and we all need to work hard to make sure the information gets to the right people,” he said.
Kane said it's important to emphasize the journey that it took for all immigrants in California to be eligible for Medi-Cal. “We know that this is a community-led, community-driven effort. That's the only reason we're doing this because people stood up and advocated for their family members and themselves,” Kane said.