At 8:17 p.m. on April 2, Dr. Luis Navazo fired off a text to the administrator of Boulder Creek Post Acute Care. Navazo heard that an employee of the Poway facility had contracted COVID-19.
The administrator confirmed as much. The prior day, the employee’s test came back positive. Frustrated, Navazo asked when the facility had planned to notify him. A geriatrician who cares for patients throughout San Diego, he visited Boulder Creek in late March, during the period when the infected employee was likely contagious.
The geriatrician — outfitted these days with equipment like an N95 mask and a gown to protect himself and others — later tested negative for coronavirus. But he believes he should have been notified about the positive test sooner, and even looped in when the facility first suspected the case.
San Diego doctors who are in and out of senior facilities say information that’s vital for doing their jobs has been tough to come by in recent weeks.
Skilled-nursing facilities aren’t explicitly required to disclose possible and confirmed COVID-19 cases to health care workers, meaning disclosure policies vary across the industry, according to industry advocates.
In addition, there are major gaps in recently published data on senior facilities with coronavirus cases, sowing confusion. This adds to well-publicized challenges like shortages of tests to tell who is sick.
In an email, Boulder Creek administrator David Gunnell said the facility immediately contacted staff, families, residents and vendors after the positive test.
“Dr. Navazo was going to also be informed as well, but he beat us to the punch by reaching out to me first to verify the case was positive, at which time he was timely notified,” said Gunnell.
Essential personnel like doctors and nurses are wary of spreading the disease among a population that’s frail and vulnerable to infection. The number of coronavirus-linked deaths in nursing homes has surpassed 10,000 nationwide, according to an April 23 tally that didn’t include some states.
Mobile doctors say being clued into the latest developments in senior homes makes for better planning — for instance, a facility with infected residents becomes the last stop of the day in a string of visits. They don additional protective gear. And they go in with a different mindset.
“If I know what’s going on and that you have an employee who tested positive or is showing symptoms, I’m now looking at my patients with more vigilance,” said Navazo, who repeatedly stated his intent is to improve the industry, not criticize.
State and federal rules require that skilled-nursing facilities and assisted-living facilities notify residents and their family members of positive COVID-19 tests. But in federally regulated skilled-nursing facilities, nothing on the books explicitly says employees and contractors must be informed as well, said Toby Edelman, senior policy attorney for the Center for Medicare Advocacy.
“I’ve heard from various residents that employees are often left in the dark because the facilities are afraid they won’t show up,” said Patricia McGinnis, executive director of California Advocates for Nursing Home Reform.
After a Voice of San Diego inquiry into employee notifications, the California Department of Social Services, which regulates assisted living facilities, on April 27 advised that health care workers also be informed of positive COVID-19 tests.
Even without directives, many senior facilities do the right thing, geriatricians say. They include employees and contractors in coronavirus updates, supply personal protective equipment, screen personnel before granting entrance to buildings and constantly clean.
But notifications can fall by the wayside. That reality, combined with incomplete data tracking facilities with COVID-19 cases, has made mobile clinics think twice before sending caregivers to senior homes.
“We’ve cut down on the frequency of our visits,” said Dr. Karl Steinberg, a geriatrician and medical director of Hospice by the Sea in Solana Beach. The wariness cuts both ways, with senior homes turning to telemedicine to reduce contagion risk, spurred by the federal government last month loosening telehealth regulations. But some need in-person care.
On April 17, the state named senior facilities with confirmed COVID-19 cases, after weeks of pressure from families, watchdogs and doctors. Earlier, Steinberg pushed San Diego County — which also holds this information — to follow in the footsteps of Los Angeles County and publish facility names.
When the county declined, local geriatricians created a WhatsApp group to share facilities with COVID-19 cases. But the list wasn’t comprehensive. That became apparent when the state on April 17 released a list of facilities with coronavirus, which is now regularly updated.
The county declined an interview request, but county spokeswoman Sarah Sweeney said while the state can release such data, the county doing so would be violating privacy laws by potentially exposing the identities of those infected with the virus.
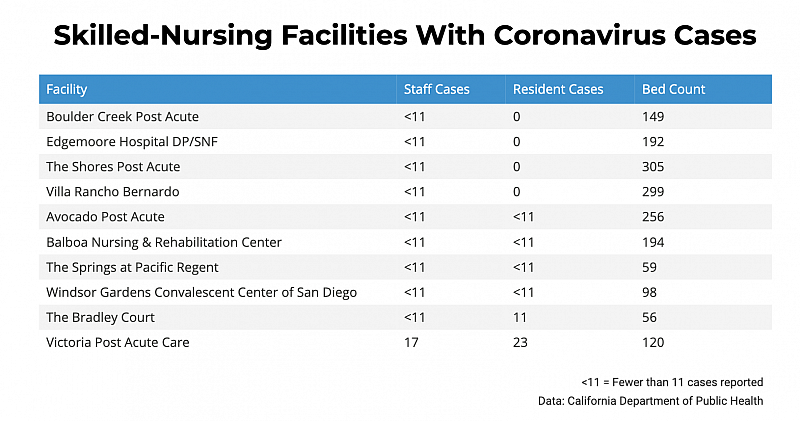
In San Diego, 10 of 72 responsive skilled-nursing facilities reported COVID-19 cases, according to state data. The hardest-hit site: Victoria Post Acute Care in El Cajon, where 17 health care workers and 23 residents tested positive. The facility has 120 beds. Fifteen nursing homes did not respond to the mandatory survey.
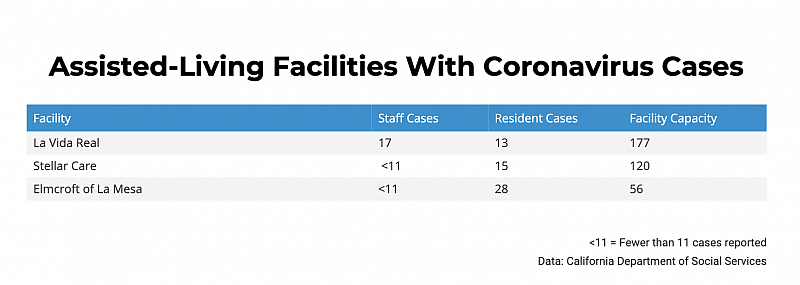
The state also released coronavirus data on assisted-living facilities, an entirely different animal. Unlike skilled-nursing facilities, the federal government doesn’t oversee assisted-living facilities. They are non-medical, often marketing themselves as more homelike than other options.
Three assisted-living facilities in the region — La Vida Real, Stellar Care and Elmcroft of La Mesa — disclosed outbreaks, per state data. But the figures omit facilities with six or fewer residents — or about 74 percent of San Diego’s 593 assisted living facilities.
The cutoff reflects “privacy and security concerns for adult and residential care facilities for the elderly, which are often private residential homes,” the California Department of Social Services said upon releasing the data.
Watchdog groups like San Diego-based Consumer Advocates for RCFE Reform criticized the decision, saying the public isn’t interested in who has COVID-19 but rather where outbreaks are, especially when making placement decisions.
Dr. Taib Rawi, a nursing home director and the owner of a San Diego-based mobile geriatrics practice, said it took too long to publicly disclose facilities with coronavirus cases. He cited the lack of transparency as a weakness in what he deemed otherwise strong county and state action to contain the coronavirus. Other doctors echoed the sentiment.
“If we’re not aware, then how do we properly protect ourselves and put in workflows so that we’re not potentially spreading it to other communities?” said Rawi.
When the outbreak began, some skilled-nursing facilities seemed wary of reporting the presence of the coronavirus, even to other providers, because no one wanted to be the first, said Dr. Daniel Given. That’s changed.
“Intercommunication between the skilled nursing network has improved,” said Given, who is a geriatric physician for Scripps Health.
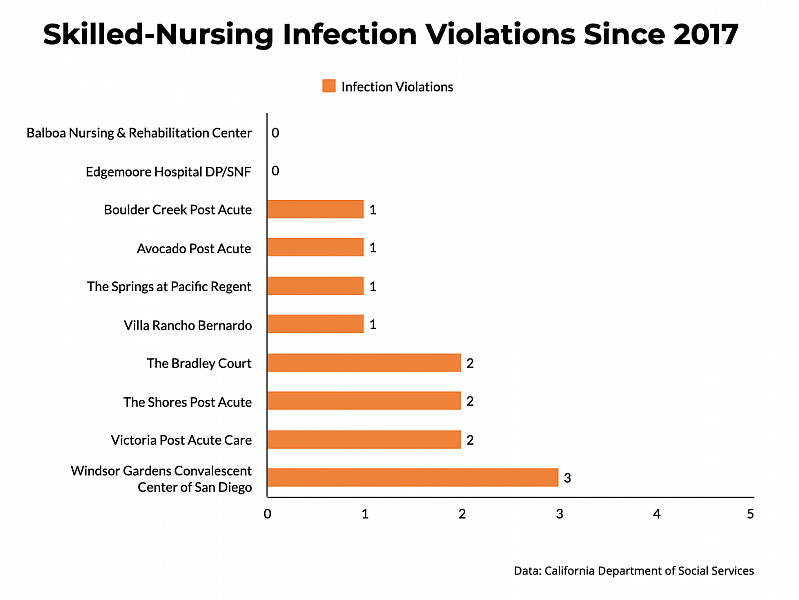
Another reason that facility data have been sought: eagerness to detect patterns, like links between coronavirus cases and facilities with poor histories of measures meant to control the spread of tuberculosis, the flu and other diseases.
Eight of the 10 skilled-nursing homes with confirmed COVID-19 cases have received at least one infection-control violation since 2017, according to a Voice of San Diego analysis.
Steinberg, the geriatrician, said there’s no “hard-and-fast correlation” between a facility’s infection-control record and the presence of COVID-19.
But, he added, a pattern of infection violations raises questions about a facility’s preparedness for COVID-19. “If a facility has a lot of deficiencies in infection control and prevention, and they’re persistent over time, that’s more concerning,” Steinberg said.
Windsor Gardens Convalescent Center of San Diego was hit with three infection violations in as many years, the most among San Diego facilities with COVID-19 cases.
In 2018, the facility didn’t report that a medication nurse had tuberculosis and then failed to determine whether other staffers were positive. This “had the potential to expose all residents in the facility,” states an inspection report.
Last year, staff hung dirty gowns on a clean washing machine, and in 2017, a nurse didn’t clean and disinfect a glucometer after resident use, according to inspection findings.
It’s unclear how many COVID-19 cases the facility has because state data lists the number of staff and employee cases as fewer than 11 — the state’s way of trying to protect privacy.
In an emailed statement, Windsor Gardens said it has collaborated with local, state and federal authorities. Residents who have tested positive remain in-house and are in isolation. Staff members who are ill are quarantining at home, the facility said.
“For some time now we have been screening employees at the start of each shift for symptoms of COVID-19 infection,” which includes temperature checks and a federally approved questionnaire, the statement says. “Employees who show signs of illness are asked to leave immediately and isolate at home.”
The Centers for Medicare & Medicaid Services nearly always classifies infection-control issues as minor violations, sparing the facility a fine or penalty. In recent weeks, watchdogs have renewed calls for tougher infection-control rules.
“An awful lot of homes have had infection violations for things that weren’t considered serious,” said McGinnis, who heads California Advocates for Nursing Home Reform. “But today, some of those violations could kill somebody.”
Besides calling for rules with more teeth, she expressed concern over the threat to an Obama-era regulation that took effect in November requiring that long-term care facilities employ an infection preventionist at least part time. Last summer, the Trump administration moved to roll back the regulation, calling it an excessive administrative burden, and instead proposed mandating only that preventionists spend “sufficient time at the facility.”
Meanwhile, assisted-living facilities face fewer requirements for infection-control procedures.
Even families who should be notified about Covid-19 cases are being left in the dark.
Margie Schroeder, whose 82-year-old mother resides in La Vida Real, found out in March that facility employees had tested positive for COVID-19 through a 10News report. She was alerted to additional coronavirus cases at the facility through a 10News report on April 16.
As of April 20, La Vida Real reported 13 residents and 17 workers with COVID-19. Schroeder said La Vida Real has gone long stretches without providing updates, leading her to question whether the facility is looking out for her mom.
“I can’t get any answers from anybody,” she said. “It’s ridiculous they’re being quiet with what’s happening.”
Given that the virus has swept through other senior facilities, Schroeder wants to remove her mother from La Vida Real and arrange for family care, a plan backed by her sister, though another family member disagrees.
The assisted living facility declined an interview request but forwarded an April 16 letter to families and residents: “Given our community’s sizable population of over 500 residents and employees, we have had a small percentage test positive for the coronavirus within our community. We are working hard to isolate those impacted in an effort to minimize the spread of this virus.”
The letter also states that in spite of testing scarcities, the facility has worked to acquire testing kits as part of a “strategic and systemic approach to test employees and specific residents.”
“Although testing reflects a moment in time, we feel this opportunity may offer you additional peace of mind,” the letter states.
Because of low industry pay, many health aides and assistants work at several facilities, increasing the risk of spreading the virus.
As one solution, Edward Schneider, the former dean of the USC Leonard Davis School of Gerontology, said the state should consider a Medicaid rate increase for nursing homes, in turn allowing the facilities to pay workers more. But he said the idea hasn’t gotten much traction, on account of a warped public view of nursing homes, many of which provide critical care, he added.
“For legislators sitting there in Sacramento, last on their priority list is paying nursing homes more money,” Schneider said. “Many of them haven’t taken a look at nursing home reimbursement, but I wish they would.”
Karen Van Dyke owns a San Diego business that places seniors in assisted-living facilities. Some are holding off on moves into facilities for now, but others don’t have the option of waiting.
She checks state lists of facilities with infected residents, reviews social services reports, citation histories and constantly checks in with contacts at facilities. Van Dyke said she doubled up on due diligence.
[This article was originally published by the Voice of San Diego.]