Researchers, community advocates address racism’s impact on Black men’s mental health
The story was co-published with the Sacramento Observer as part of the 2024 Ethnic Media Collaborative "Healing California."

Doctor talking to ex-soldier suffering from severe headaches and faints following traumatic injury
Credit: Getty Images
George Floyd wasn’t suffering from any mental episode when he was killed by a white Minneapolis police officer, but after his May 25, 2020, death went viral, his name became synonymous with demands for better treatment, better health outcomes and better support services. His death was yet another stark reminder that America still has its proverbial knee on a brotha’s neck.
Floyd’s last words, “I can’t breathe,” eerily echoed those of two other unarmed Black men: Elijah McClain, who died after being roughed up and drugged by officers in Aurora, Colorado, in 2019, and Eric Garner, who was killed by a white New York police officer in 2014 for allegedly selling loose cigarettes. The three-word plea may have initially fallen on deaf ears, but would then resonate and reverberate around the globe, becoming a rallying cry for Black men who, for centuries, have been choking under the weight of systemic racism and discrimination.
The deaths of these men, and countless others whose names have been added to a growing list, has forced people to look at ways Blacks, particularly Black males, are suffering. Mental health is at the top of the list.
Dr. Ruth Shim, a professor of clinical psychiatry in UC Davis’ department of psychiatry and behavioral sciences, says she was initially optimistic about the attention and vehemence that came after Floyd’s death.
“When George Floyd was murdered, I felt very strongly like there was a window, a tiny window of opportunity where people cared about this issue. I knew just based on the history of this country, that that window would close very, very shortly. The window stayed open longer than I expected it to, but it has closed,” says Dr. Shim, who also serves as the local university’s associate dean of diverse and inclusive education.
“We’re almost four years after the murder of George Floyd and we see DEI [diversity, equity and inclusion] and any interventions to try to improve equity and health equity, completely under attack.”
A nonprofit called Do No Harm, which calls DEI a “divisive trend in medicine,” recently moved to block UCLA’s medical school from teaching students about racism and its impact on health through a widely used practice called racial caucusing, or separating into groups based on levels of comfortability.
Dr. Shim finds efforts to “police medical schools” disturbing.
“I thought, after George Floyd’s murder, that we finally had a pendulum swinging in a direction where we were going to try to address equity and mental health equity, and the fact is, these outcomes for Black people are so much worse than almost every other population,” she says.
With attacks on affirmative action and critical race theory, and lawsuits against organizations that work specifically to help Blacks reverse long-term effects of marginalization on the rise, the country seems to have gone in a different direction entirely, Dr. Shim says.
“It’s not just Do No Harm, it’s the Supreme Court,” she adds. “It’s everybody that is of the belief that ‘we’ve done all we need to do around addressing issues related to race and now it’s time to make sure everybody gets the same opportunities,’ and ‘we’re really focusing on fairness and that we’re not adversely benefiting one population over another.’
“I would agree with that if the outcomes for those populations were equal. But we see terrible, terrible differences in outcomes for Black people compared to white people. We see really bad outcomes and particularly in mental health.”
State Of Mind
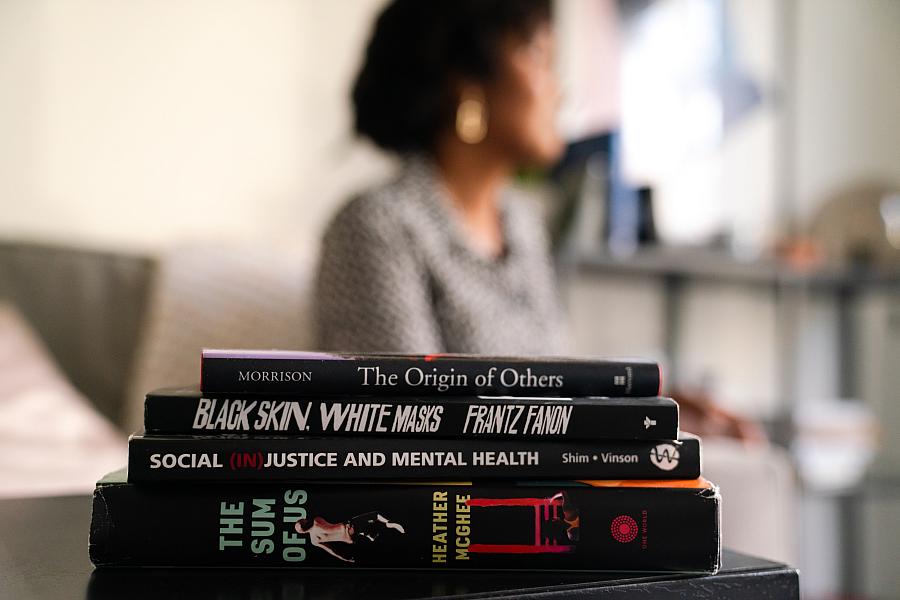
UC Davis researcher Dr. Ruth Shim studies the impact of racism in healthcare. Russell Stiger, Jr., OBSERVER
Credit: Louis Bryant III
President Joe Biden addressed the nation’s mental health crisis in his first State of the Union address in March 2022. It was two years into the COVID-19 pandemic and President Biden spoke of the American people being driven to a “breaking point” dealing with grief, trauma and isolation. He outlined a strategy to “transform how mental health is understood, perceived, accessed, treated, and integrated.”
“Our country faces an unprecedented mental health crisis among people of all ages,” President Biden said. “Two out of five adults report symptoms of anxiety or depression. And, Black and brown communities are disproportionately undertreated – even as their burden of mental illness has continued to rise.”
Gov. Gavin Newsom also vowed to make mental health a top priority. Gov. Newsom promised to modernize and transform the state’s mental health system into one that “meets the needs of all Californians.” He is spearheading what he calls “California’s Mental Health Movement” and has signed Senate Bill 326, updating the Mental Health Services Act, and Assembly Bill 531, a $6.38 billion bond to fund construction of new behavioral health housing and treatment settings across the state. Californians will vote on Prop. 1, which seeks to address multiple crises – mental illness, substance abuse and widespread homelessness – on March 5.
In December, the California Department of Health Care Services awarded $150 million in grants to 262 organizations to support the mental health and wellness of young people. Of that amount, $100 million was designated for programs that support youth by mitigating the effects of adverse childhood experiences (ACEs).
“We see the signs of our broken system every day – too many Californians suffering from mental health needs or substance use disorders and unable to get support or care they need,” Gov. Newsom said in October.
A Heavy Burden
Black men often say they feel as if they have the weight of the world on their shoulders. The overall stress of Breathing While Black can take its toll. Some decide that it’s just “too much.”
According to the U.S. Centers for Disease Control and Prevention, the death rate from suicide for African American men in 2018 was four times greater than for African American women. The CDC also listed suicide as the third leading cause of death for African Americans males ages 15 to 24. The suicide rate for African Americans rose by 19.2% between 2018 and 2021 and another 3.6% from 2021 to 2022. The rate for all men increased 2.3% in that period. Experts say fallout from the COVID-19 pandemic and other everyday social determinants of health, including racism, discrimination, poverty, lack of educational opportunities, and limited access to physical and mental health care, played a role.
Studies show racial trauma can increase the risk of Black people meeting the criteria for post-traumatic stress disorder, as hormones are released during stressful situations, such as experiencing and observing racial discrimination. Being constantly stressed can result in chronic diseases such as high blood pressure and heart disease, as well as mental health conditions like depression, anxiety, and other chronic illnesses that disproportionately plague the Black community. In 1992, Dr. Arline Geronimus, a health researcher at the University of Michigan, coined the phrase “weathering” to describe the deterioration of Black people’s health from chronic stress of racism.
Sankofa
Researchers and community advocates say any attempts to address mental health in the Black community must acknowledge the historical role race and racism has played.
“In order to plant seeds for systemic change, equity, inclusion and cultural competency, we must study and examine oppressive historical structures which negatively impact people today,” says Sandy Holman, author and founder of the Culture C.O.O.P.
“This lays the foundation for creating new ways for people to view and engage with one another.”
Failure to look back and reclaim power over a false narrative is a recipe for disaster, Holman says. The powers that be, she continues, devalued Black people to justify enslavement and continue the practice today to give grounds for gross mistreatment.
“Mix in control over all major institutions such as media outlets, government, economics, the criminal justice system, education, environment, health care, where one can live, and anything that affects a person’s ability to survive and thrive, to build an incredibly efficient, interconnected means of generational oppression, incredible hardship and disproportionate death, among targeted groups. All the aforementioned is essential to control the narrative, from micro to macro levels, and ensures a dysfunctional mindshare among the masses in how we perceive certain cultural groups,” Holman says.
In Dr. Joy DeGruy’s 2005 book, “Post Traumatic Slave Syndrome: America’s Legacy of Enduring Injury and Healing,” New York-based television producer and host Gil Noble calls slavery a “400-year-old abscess that remains unhealed.” In the book, republished in 2017, Dr. DeGruy discusses the impact of American slavery on the Black psyche.
“The slave experience was one of continual, violent attacks on the slave’s body, mind and spirit,” writes Dr. DeGruy, a former mental health clinician and university educator. “Slave men, women and children were traumatized throughout their lives and the violent attacks during slavery persisted long after emancipation. In the face of these injuries, those traumatized adapted their attitudes and behaviors to simply survive and these adaptations continue to manifest today.”
Dr. DeGruy’s work addresses the long-term psychological and emotional effects racism and discrimination have had on the Black community and suggests that many of the symptoms and behaviors resulting from that continued trauma, such as low self-esteem, stress, self-sabotage. violence, substance abuse and absenteeism, can be attributed to PTSS, a concept she coined.
Mass media often is blamed for perpetuating and projecting negative images of Black men and boys as ignorant, violent and criminal-minded. It’s also accused of presenting whiteness as the standard for beauty, wellness and overall success.
“What is not addressed is the role our history has played in producing these negative perceptions, images and behaviors,” Dr. DeGruy writes. “We rarely look to our history to understand how African Americans adapted their behavior over centuries in order to survive the stifling effects of chattel slavery, effects which are evident today.”
Racism Is Bad For Your Health
Mental Health America, a national nonprofit dedicated to the promotion of mental health, well-being and illness prevention, says racism and bigotry are “just the tip of the iceberg,” pointing to how Blacks and other people of color are often subjected to “more subtle traumas” such as witnessing high mass incarceration of others in their areas; having white neighbors call law enforcement on them for simply standing in front of their own homes, minding their own business; attempts to erase their history from school curriculum; and having banks and credit institutions refuse to lend them money or when they do, it’s at higher interest rates.
Change starts with education and understanding, but sadly, Dr. Shim says, there has been a historical disconnect. Mental health care in this country, she adds, always has operated in an apprenticeship-like fashion.
“You learn how to become skilled in mental health care by learning from other people. The people who have traditionally taught and trained providers have usually been white people, mostly white men, and so they are using their frame of reference for identifying problems, conceptualizing why people behave the way they do,” Dr. Shim says. “Because white men in this country are less likely to be oppressed, they don’t have a frame of reference for how oppression impacts health and health outcomes and mental health outcomes, so they can’t teach about something if they have no concept of it and they don’t know.”
Racism and cultural ignorance in the medical field have had dire consequences.
“It’s really common for psychiatrists, especially 20 years ago, to misinterpret distrust of the police as a paranoid perspective, particularly with Black people,” Dr. Shim says. “For example, if a Black man says he doesn’t feel like the police support him or protect him, that might be viewed as a paranoid thought or a thought like that might be seen as a mental health problem. Then you’re more likely to say, ‘Oh, this person has paranoid beliefs and maybe these paranoid beliefs rise to the level of schizophrenia.’”
Schizophrenia often is overdiagnosed in Black men, who are four times more likely to be diagnosed with the disorder than their white male counterparts. Dr. Shim points to “The Protest Psychosis: “How Schizophrenia Became a Black Disease,” a book by white psychiatrist Jonathan Metzl, that outlines how the disorder went from being considered non-threatening to being weaponized against a group of people.
“Prior to the 1960s, they were diagnosing schizophrenia mostly in white women who weren’t ascribing to the standards of society. If they didn’t want to take care of their children and if they didn’t want to obey their husbands, they would get diagnosed with schizophrenia and they would be sent to a hospital and they would stay there for like a year or so,” Dr. Shim says. “Then the civil rights movement started and these white psychiatrists started changing the definition of schizophrenia to associate it more with psychotic, paranoid beliefs. They misinterpreted people fighting for civil rights as being hostile, aggressive people who were paranoid and had delusions and false beliefs about white people being harmful to them, and an ideology against white people.
“These beliefs were published in a 1968 journal article, talking about protest psychosis and describing the features of this particular illness. That completely transformed the hospital; they started hospitalizing Black men against their will, during the rise in civil rights. That increase in defining schizophrenia and changing schizophrenia to be more of a hostile, paranoid problem of Black men really led to the increased diagnosis of schizophrenia in Black men for the next 40-50 years.”
If hospitalizing people for standing up and speaking their minds was the lay of the land today, hundreds of thousands of Black people would have been admitted for protesting the deaths of Floyd, Breonna Taylor and locally, Stephon Clark.
“It’s so scary because what this book really talks about is how psychiatry has been used as a means of social control, as a means to remove ‘problematic individuals’ from society,” Dr. Shim says. “Metzl’s argument in this book is that society, white society in particular, had this perspective that Black people fighting for their civil rights, particularly Black men, were a threat. Then they employed these methods to remove that threat from society by hospitalizing all of these Black men and taking them out of the population, so that they could not ‘harm people.’”
Stressed Out

Dr. Troy M. Williams helped create the local barbershop support effort, Cut to the Chase, wanting to give Black men a safe space to address their mental health and well-being.
Courtesy photo
Researcher Dr. Troy M. Williams mentions the harm many experienced after the very public law enforcement-involved deaths of Eric Garner, Trayvon Martin, Oscar Grant, and Michael Brown – and the lack of accountability for their killers – in the abstract to his 2015 thesis, “Good Kids, Bad City: The Examination of Crime Resistance in Low Income, High Crime, Communities of Color.”
“The death of these men has drained me, left me feeling hopeless and afraid of law enforcement,” Dr. Williams writes.
His paper, which takes its name from a 2012 album by conscious rapper Kendrick Lamar, was written at the University of San Diego and studies men of color who resisted assimilated criminological behavior. Dr. Williams sought to dispel the myth that all Black men from high crime areas commit crime and address the “unconscious racist practices that block the full integration of Black men into mainstream society.”
The men in Williams’ research were not too unlike those he saw growing up in College Park, a lower-middle-class neighborhood in Atlanta.
“Many of the criminals and non-criminals I spoke with just discussed with me the stresses that they deal with and navigate, a lot of those being economic reasons,” he says.
Dr. Williams created a documentary on his research and began to see that much of what the men were experiencing overlapped into mental health.
“Negative images of Black males have caused African Americans to internalize self-doubt and have influenced their behavior in many different settings,” Dr. Williams writes.
The documentary got him noticed by several doctoral programs and landed him at the University of Wisconsin, Madison. Today, Dr. Williams is chief impact officer for the Greater Sacramento Urban League. He’s also the co-creator of Cut to the Chase, a mental health support group that meets at local barbershops.
Hope For The Future

Local nurse and Black men’s health advocate Aron King, center, and Ronnie Cobb of the Greater Sacramento Urban League, left, share a light moment during a Cut to the Chase event.
Seth Patterson, OBSERVER
“We have all suffered from our ignorance around mental health and it’s always such a thin line between mental health crisis and it being a public health outcome,” says Madalynn Rucker, founder and executive director of OnTrack Program Resources, a local social justice organization dedicated to eliminating disparities through community-centered approaches to health and wellness.
“There are other issues that are happening in the community, so our disparities are so complex. It’s hard to just point to mental health,” Rucker says. “It’s also the politics, the general health and the historical crisis that we’ve been in for a long time due to the basic racism and the history out here. It’s day by day. It’s putting one foot in front of the other and recognizing how things are linked together. We have to do that in order to figure out how to unlink them and address them.”
Knowledge must lead to action, Rucker says.
“Complaining all the time and calling folks out with no progress and no action plans, often guides us to somewhere else,” she says. “Mad ain’t enough.”
According to the U.S. Department of Health and Human Services, “achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities.”
Dr. Shim admits to being overwhelmed in the past, feeling responsible for “fixing it all.” Her thinking has shifted.
“I feel like my responsibility is to train and ready the next generation of people to solve these problems,” she says.
It’s an awesome charge. Educating those who will come behind her, gives her room to be hopeful.
“I consider myself to be a skeptical optimist. I can’t say we’re losing the battle. The optimist in me thinks that one of the reasons the opposition and the retrenchment is getting so powerful at this moment, is because we’re getting very close to breaking through in terms of really addressing these issues. That’s kind of a way that I remain optimistic.”
This Sacramento Observer project is supported by the USC Annenberg Center for Health Journalism, and is part of “Healing California,” a yearlong Ethnic Media Collaborative reporting venture with print, online and broadcast outlets across California.
