Asians with Postpartum Depression Need Better Perinatal Care
The story was co-published with AsAmNews as part of the the 2024 Ethnic Media Collaborative, Healing California.

Comedian, actress and postpartum depression survivor Jiaoying Summers with her 4-year-old son and 2-year-old daughter in their home just outside of Los Angeles. Photo by Dustin McWethy
During her sets, Jiaoying Summers, a Chinese American comedian, jokes about the time she drove to a beach in Malibu and swallowed a bottle of Ambien.
While waiting for the drugs to take effect, she texted an old friend to seek forgiveness for not treating him better when they were younger. He called her and persuaded her to chug a two-liter bottle of water while sticking her finger down her throat.

Jiaoying Summers. Photo by Dustin McWethy
Summers narrowly escaped death due to postpartum depression (PPD), a mental health condition affecting up to 20% of mothers around the world and 10% of fathers.
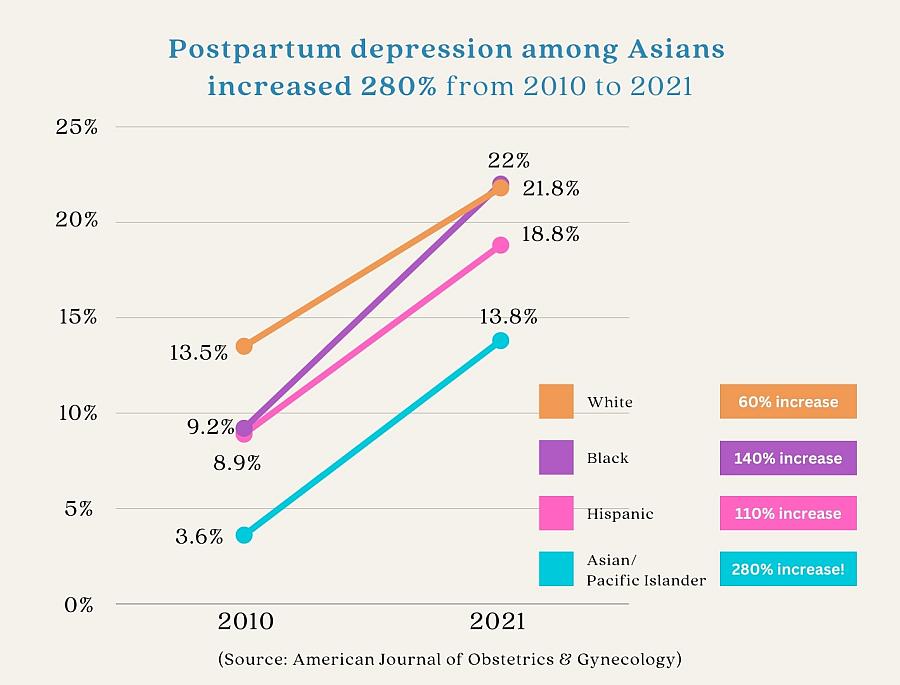
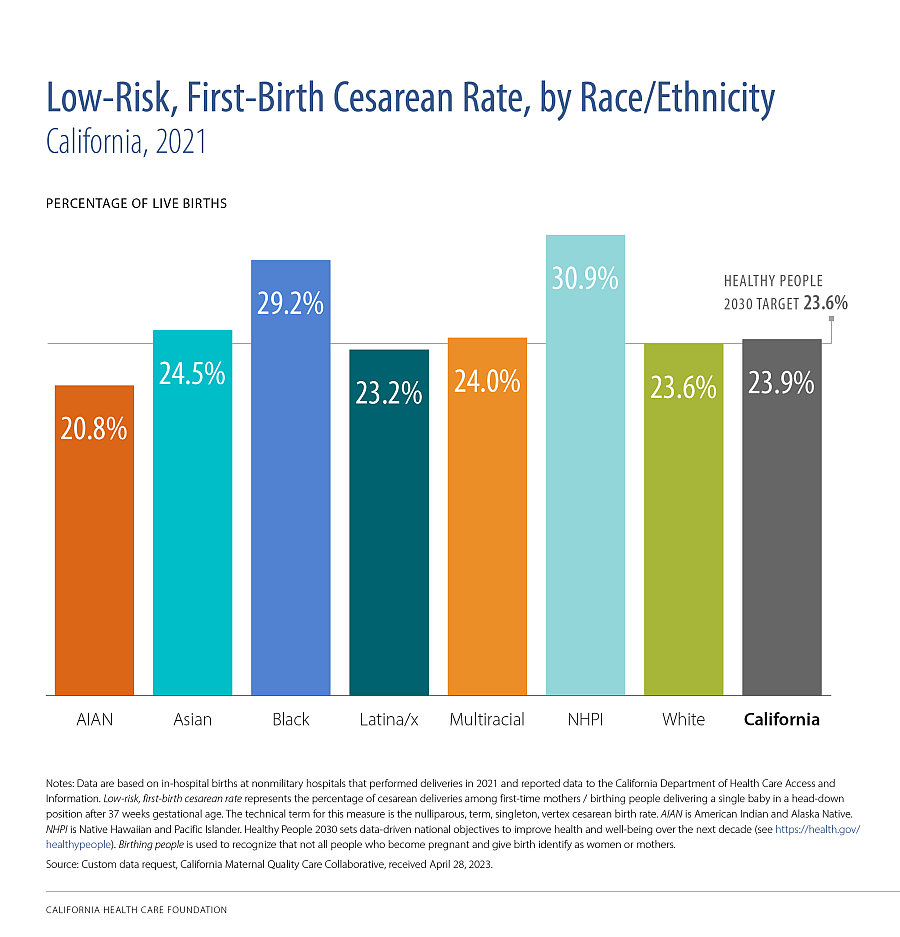
In California, diagnosis of PPD has increased dramatically in Asian communities, and nationwide, Asian and Pacific Islander women are at higher risk of PPD compared to White, Black and Latino women. Against a backdrop of high rates of C-section interventions, there are few culturally competent birthing and postpartum professionals, and lower awareness of how to access the resources that exist.
Summers considered herself an extremely strong person, maybe second only to her mother. But lack of emotional support networks, an abusive domestic environment, the struggle to succeed as a comedian and actress, plus financial dependence on her then-husband wore on her mental health and placed her at heightened risk for PPD.
After her first child was born, she had told her then-husband that she needed help because she was very sad and had never felt this way before. His response was that she was selfish — she had every reason to be happy, and only crazy people saw therapists.
Summers said that if she had been contending with just one of these hardships, she would not have been driven to the edge. She made the attempt on her life about six months later.
“The moment I threw up, I was like, what the fuck? Wow, I went there,” Summers said on a Sunday in January, in her Southern California home.
‘I needed to be better yesterday’
A Centers for Disease Control and Prevention (CDC) study estimated that 1 in 8 women reported postpartum depressive symptoms in 2018, and the Pew Research Center found that from 2008 to 2019, about 1 in 11 women aged 15-44 who “succeed” in killing themselves were pregnant or had recently given birth.
Symptoms of PPD include feeling intensely sad, anxious, overwhelmed, fatigued, hopeless, resigned, detached or unable to care about or love one’s baby. The signs of PPD commonly appear within six weeks of a baby’s birth but can show up at any point during pregnancy and up to a year after giving birth.
PPD is more severe and persistent than the “baby blues” of anxiety, stress, insomnia, loss of appetite and crying spells up to two weeks after giving birth due to fluctuating hormones.
The worst consequences of untreated PPD can include psychosis (loss of reality and imagined situations), infanticide and suicide, the leading cause of death for women during pregnancy or within a year of having given birth.
A 2023 study of Kaiser Permanente Southern California’s electronic health records found that PPD among Asians increased 280% from 2010 to 2021 — the highest relative increase of any other ethnic group.
Graphic by Bailey Franzen
The death of 31-year-old Nima Bhakta by suicide in August 2020 was part of this rise of PPD in Asian communities. Bhakta, who was of Indian origin, left behind a 7-month-old son and other family members and had posted messages pleading with the public to not blame anyone, least of all a society that did not understand PPD.
South Asian physicians across the country put together a Facebook video sharing their own experiences to help others detect PPD: Extreme changes in appetite. Explosive anger followed by immense shame. Avoidance or other isolating behavior, whether physically removing oneself from others, refusing to converse about hardships or lashing out at people trying to offer help or resources.
Jasmine, who withheld her last name from AsAmNews because of career privacy concerns, had a low-risk pregnancy followed by a standard birth experience.
Postpartum depression soon obscured her initial joy. On one occasion, she could not descend a set of stairs without sitting down to weep.
She obtained a prescription for antidepressants. But as a pharmacist, she knew how long the drugs took to work. I needed to be better yesterday, she thought.
Eventually, Jasmine connected with a psychiatrist who helped enforce a sleep schedule and prescribed medication that “lifted the fog” just enough so she could continue getting help.
Last August, the U.S. Food and Drug Administration approved Zurzuvae (zuranolone), the first oral treatment targeting PPD. The pills, taken twice a day “with a fatty meal,” promise to alleviate PPD in as few as three days. However, the drug remains hard to access, and does not cure life’s circumstances.
“I personally think all moms who are pregnant should be connected with a therapist who knows them,” Jasmine said, adding that it takes time to find and build a relationship with the right match.
“If you think it’s going to be hard work to find somebody, don’t you think you should start sooner in pregnancy rather than later after you give birth?” she said.
Stigma, or lack of access?
CDC data determined that 80% of the pregnancy-related maternal deaths across 36 states from 2017–-19 — including lives lost due to mental health consequences — could have been prevented.
Public health messaging to raise awareness about PPD has focused on letting people experiencing PPD know that they are not alone, that their symptoms will not last forever and that they must seek mental health treatment.
Asian people with symptoms of PPD remain among the least likely to receive, seek out or access mental health help. Outreach literature repeatedly cites the stigmatization of mental health topics by Asian cultures as a chief reason for the gulf between the problem and the solutions.
“It goes far beyond stigma — it’s access, it’s language. Stigma isn’t always in the room when it’s just me relying on my doctor and care,” said Estella Owoimaha-Church, the executive director of Empower Pacific Islander Communities (EPIC) based in Southern California.
Owoimaha-Church, of Samoan and Nigerian heritage, was so concerned with preventative maternal care that she visited Planned Parenthood when she was in her early twenties, long before thinking of having kids. The counselor told her the best thing she could do for herself if she ever became pregnant was to find a therapist.
Once ready to try for a child, she visited an OB/GYN at Cedar Sinai in Beverly Hills, Calif., hoping to find higher-quality care in that neighborhood. The Asian doctor told Owoimaha-Church that she was morbidly obese and would not be able to conceive until she lost weight.
“It was full of shame, it was fat-phobic, it was anti-Black,” Owoimaha-Church recalled.
Six months later, she was pregnant. Soon after giving birth, she went back to her high-stress teaching job and blamed herself for not feeling better fast enough. She could not find a culturally competent therapist she liked and trusted, and she lacked the type of insurance coverage that could help her afford treatment.
Hips too small, cut in half
The U.S. Office of Women’s Health states that women who have had traumatizing births or problems with a previous pregnancy or birth could be at higher risk to encounter PPD.
Asian people undergo some of the highest rates of physically and emotionally traumatizing C-section birth interventions.
A recent article by Scientific American reported that the average C-section rate in the U.S. held steady at 33% between 1997 to 2021, amounting “to about half a million unnecessary surgeries every year” despite the procedure posing a 3.6 times higher risk of maternal mortality.
According to the March of Dimes association, the national average C-section rate from 2020–22 was 32.9% for Asian and Pacific Islanders, the second highest after Black women at 36.3%.
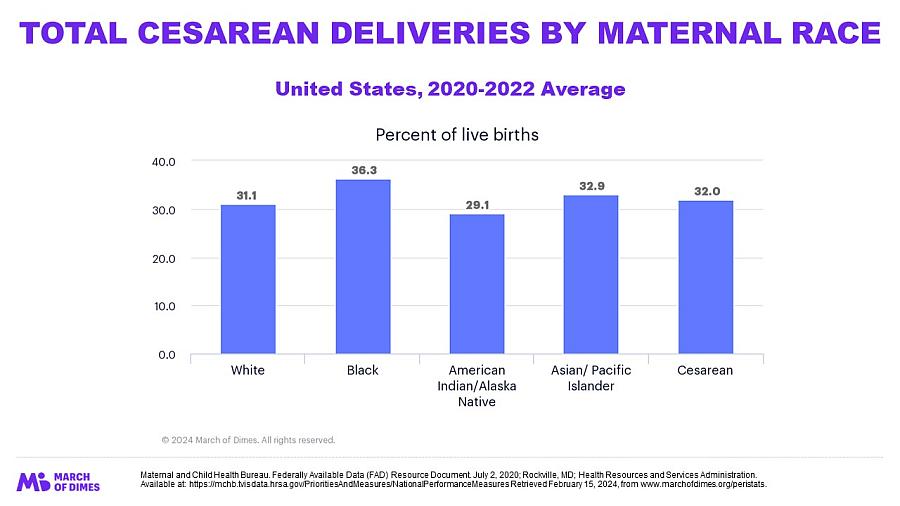
In California, the average C-section rate for Asian and Pacific Islanders was lower than the national average at 30.9%.
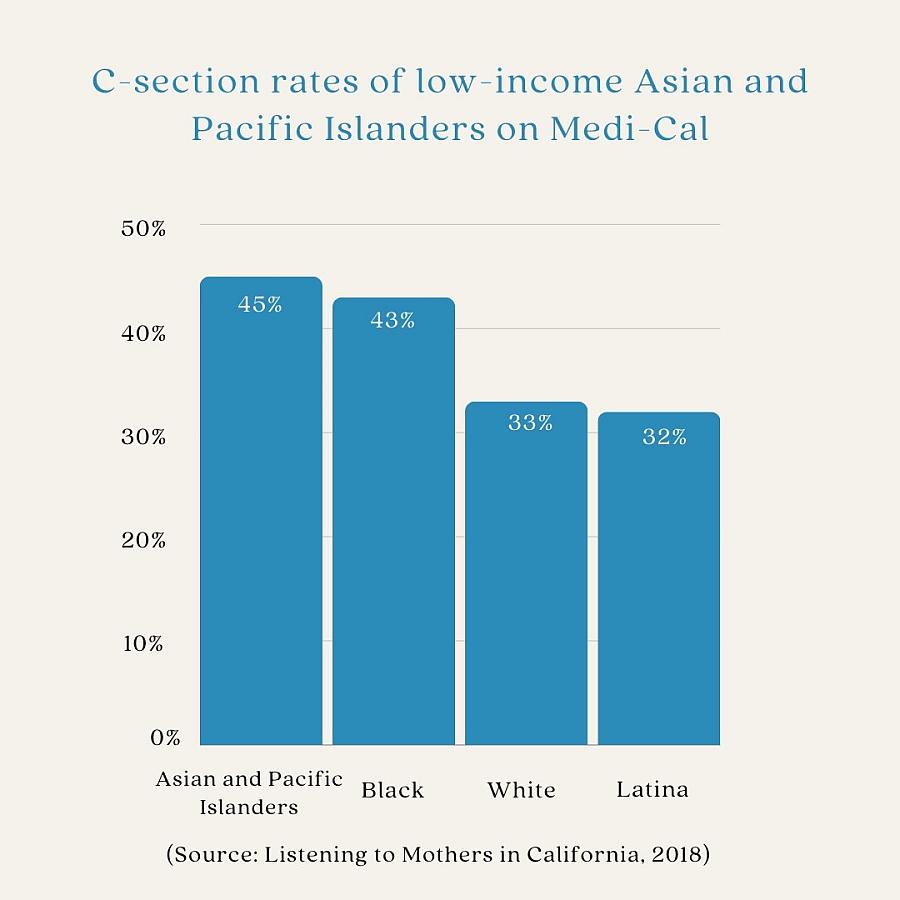
However, the Listening to Mothers in California report of 2018 found that C-section rates of low-income Asian and Pacific Islanders on Medi-Cal, California’s Medicaid public insurance, were the highest for any group at 45%, comparable to the rate of 43% for Black people in the program.
Graphic by Bailey Franzen
Disaggregated data from the 2023 edition of the California Health Care Foundation (CHCF) Maternity in California report revealed the health disparities that Native Hawaiians and Pacific islanders face when it comes to C-section rates. Native Hawaiians and Pacific islanders had the highest C-section rate for low-risk, first-time births out of any other ethnic group.
Singaporean Peranakan Chinese Bay Area resident Cherie Seah was close to becoming a maternal health statistic when she had her second child at age 33 in 2018 at the Kaiser Permanente hospital in Oakland, Calif., with a doula present.
When she thought she was pushing, the doctors told her that the baby’s heart rate was slowing down and that she had to have an emergency C-section.
“When you think your baby might die because that’s how they put it across to you … my first reaction was to save my baby,” she said.
Instruments clattered as the team converted into a surgical squad. As the clinicians began wheeling Seah into the operating room, her doula whisper-shouted into her ear, “Cherie, you push this baby out.”
This brought Seah back into herself, to a sense of autonomy.
Without waiting for permission, she pushed during her next contraction. Her baby was born.
Now a doula herself, Seah owns a pelvic floor model, which she uses to show clients that when a baby is “stuck” in the birth canal, it is not because Asian women’s pelvises are too small to have their babies.
“When it comes to maternal health, there’s an acceptance of these high numbers. Why?” asked Seah, in regard to emergency interventions.
Obstetrician Dr. Nancy Z. Tang, M.D. FACOG, who works in Dublin, Calif., said that she does observe more petiteness in Asian women in areas such as the introitus, the entrance to the vagina, or the perineum between the vagina and anus.
But the risk of a baby getting “stuck” is determined before birth, using pelvimetry. These screenings determine whether the size of a baby’s head is approaching the 10-centimeter extent of how much a “ripened,” or opened, cervix can dilate during labor.
In that case, the doctor has the choice of scheduling a C-section or inducing labor.
When it couldn’t have been any other way
On balance, interventions like C-sections, episiotomies (the use of surgical scissors to cut an extension into the opening of the vagina to help a baby come out) and vacuum extraction to aid delivery have kept women and their babies from dying. Some rural or underserved areas struggle to access these procedures.
However, people who have undergone interventions may benefit from more physical and mental aftercare than the standard procedure of sending new parents home with a pack of adult diapers and instructions to schedule a follow-up appointment in six weeks.
Cindy Lim, in her mid-forties, is a naturalized Korean American woman who had her first baby six months ago at Alta Bates Summit Medical Center in Oakland.
Lim, who asked to be identified by a pseudonym, had separate birthing and postpartum doulas lined up to support her goal of natural childbirth.
Her pregnancy was considered high-risk, and the maternal fetal medicine specialist anticipated that her baby would be large based on algorithms from ultrasound measurements in her third trimester. Lim had also developed preeclampsia (high blood pressure during pregnancy) the week of her due date.
Doctors induced her labor using a drug called Misoprostol and placed her in a unit with a bathtub. The hot water soaks provided so much relief when her body went into labor that she begged to give birth there.
But, per policy, the clinicians put Lim on her back and gave her Fentanyl to help her sleep before the pushing stage of labor.
When Lim’s cervical dilation stalled at seven centimeters, she received a massive infusion of an oxytocin varietal called Pitocin. She also had an epidural — a shot of anesthesia into the spine.
The outer limit for pushing is usually two hours, but she kept trying. Two hours turned to six, and her baby receded back up into her birth canal twice in a phenomenon called “turtling.”
The baby’s heart rate did not recover fast enough, and doctors ordered an emergency C-section. When the surgeons removed her son from her body after two full days of labor, Lim could not touch him because of the surgical partition placed high up on her chest.
At risk of having postpartum hemorrhage, Lim remained in recovery at the hospital for nearly two weeks while struggling to feed her baby. Her body had swelled so much that she could not recognize herself in the mirror.
Halfway to her six-week follow-up, she developed an infection in her C-section wounds and went to the hospital to obtain antibiotics. Doctors did not flag her for her birth trauma or the postpartum depression she felt she was experiencing at certain points. Symptoms of postpartum PTSD that she reported included flashbacks, fear of dread in entering hospital environments and a feeling of detachment from her newborn.
The hospital did administer required postpartum depression surveys and give her printouts of mental health resources. But Lim said she wished that connections to the specialists she needed had just been embedded into her regular maternal care.
“When you’re a new mom, especially when recovering from birth complications, it’s so overwhelming just to do basic things,” she said.
Lim’s BIPOC postpartum doula assisted with the most immediate needs of sleep scheduling and breastfeeding. This arrangement freed Lim to tend to the rest of her life, motherhood and mental health.
“I loved her — I still love her,” said Lim while breastfeeding her son in the semi-darkness of her living room.
Filling in the white spaces: Asian representation in maternal care
Lim found her life-saving care through the recently formed resources BIPOC in the Bay and the Asian Birth Collective (ABC), a network that Seah co-founded.
Seah prefers the word “birthworker” rather than “doula” and “birthing person” for a person who has a baby because not all people who give birth identify as women or as mothers.
Doula is the Greek word for “slave,” applied by medical anthropologist Dana Louise Raphael in 1976 to non-medical perinatal caregivers.
When Seah entered her first doula training session, she saw only two other Asian people in a room of about 40 aspiring doulas and started the ABC with them.

Cherie Seah: doula, mother, PPD survivor, and co-founder of the Asian Birth Collective. Photo by Earthshine Doula & Photography
The ABC network has become a hub for Asian birthworkers and birthing people across the country and around the world, with licensed clinical social workers, psychiatrists, psychologists, pharmacists, pelvic floor therapists, night nurses, lactation consultants and midwives who can legally deliver babies within or outside of hospitals.
Seah said she has found only about 10 certified Asian midwives in the Bay Area of California so far.
She has also been collecting Asian birth stories so people can see one another and get connected to resources before they need them.
“Preventative is talking about it. Preventative is sharing our stories. Preventative is about knowing our rights, and that’s why representation is important,” said Seah.
“To find someone who looks like you — that is so huge. Otherwise, I’m the failing Asian,” Jasmine echoed. When she was recovering from her PPD, she began looking for stories on Motherhood Understood, a site bought by Motherly. “I was wondering if there was anyone on here that looks like me,” she said.
She also reconnected with her Taiwanese American friend Peggy Chen and created “Healing the Tigress,” a podcast featuring in-depth conversations with maternal health professionals and people who have given birth about the interaction between maternal healthcare, mental health and Asian identity.
Cultivating awareness of postpartum care for Asian communities
Chen, who migrated to health tech after working in the inpatient psychiatric ward of the San Francisco General Hospital went on to become a certified breastfeeding peer counselor. Now, with a decade of experience as a licensed clinical social worker (LCSW) under her belt, she is working on earning her perinatal mental health certification.
When asked why she thinks her ethnic group might not speak out or seek help even in the presence of these resources, she said that she personally had not seen examples of anyone asking for help when she was growing up.
Divya Kumar LICSW, Sc.M., PMH-C, fell into perinatal support and then social work from a background in reproductive justice after her own experience with postpartum depression and anxiety.
Now specializing in perinatal mood and anxiety disorders, Kumar pointed out the power of weaponized gratitude, which she describes as growing up under the parenting refrains of “We came here with nothing, you have everything, you just need to be grateful - pull yourself up by your bootstraps.”
Kumar said that the martyrdom of the mother is an example of immigrant narratives that glorify suffering and sacrifice. And stigma manifests as distrust of the need for mental health care from people not viewed as “real doctors.”
She laughed that, as a licensed independent clinical social worker (LICSW), fellow Indians were unsure of what to make of her title as she was not a medical doctor.
“Why are you going to talk to somebody outside the family, this isn't something that we do? This is weird and indulgent — something that the soft white ladies do,” Kumar said, voicing some of the sentiments she has heard in her community.
Jasmine also cited the resilience of immigrants and their descendants, which might have helped them survive adversity while also leading to the tendency to try to tough something out alone instead of getting help.
“You don’t complain, you keep on keeping on. Our parents don’t complain; they had it way worse than we do,” she said.

Licensed independent clinical social worker and certified perinatal mental health specialist Divya Kumar, who has coordinated South Indian interest postpartum support groups. Photo by Michelle Schapiro
Kumar said, “When people ask me about Asian culture, I respond by asking, ‘What is “our culture” in the United States after immigration, intergenerational trauma, racism, forced migration, war, partition, all of those things.’ Our culture — it's not just ‘Asian culture.’ I think that's so reductive, because our behaviors are shaped by this larger socio-historical context.”
She also wondered, “What is the role of how we, Asian Americans in this country, are put in this weird hierarchy where we are supposed to behave in a certain way, and we are boxed in, and we're sort of invisible and visible in all of the wrong ways? We’re invisible in plain sight, right? How does that affect our help-seeking behaviors?”
Finally, she questioned where the culturally responsive resources were for Asians who screen positive for PPD risk prior to giving birth or are diagnosed with it afterward.
“Oh, Asian Americans are the least likely group to seek help? Seek help from whom? There's two parties here, right?” she asked.
In regard to maternal mental health, cultural gaps come into play when discussing the question of sleep training a baby so parents can get sleep themselves, or feeding a baby with formula because the breastfeeding process is not working smoothly.
“We’re not used to putting ourselves before others,” Jasmine said.
However, problematizing the lack of help-seeking by Asians takes away attention from times when Asian people speak up and are brushed aside — an experience resonant with many people of color who have had children.
In 2017, Isabel Nguyen was in therapy for the first time in her life after a mental health screening survey during a routine checkup flagged her for anxiety. She had also participated in Kaiser Permanente’s birth education training programs very early on in an effort to be prepared.
However, she went into labor sooner than expected and had an emergency C-section for her breech baby at the University of California, San Francisco Medical Center. More than 10 clinicians at the teaching hospital were involved in pulling her baby back out of her birth canal, up through her uterus and out of her body.
Afterward, she started feeling feverish and chilly. She was convinced that she had an infection.
Her mother, a Vietnamese immigrant who trained as a labor and delivery nurse, among other specialties, and provided health services and Vietnamese language interpretation for poor, single, underaged mothers and their infants in Southern California, also diagnosed Nguyen’s condition as an infection.
Mother and daughter repeatedly told a floor nurse, who happened to be white, that the symptoms indicated infection. They requested medical attention.
“Wow, are you a doctor?” the nurse asked before telling the two women that this was all normal after a C-section and that they should be strong.
Hours later, Nguyen developed a fever and entered emergency treatment for sepsis due to E. Coli exposure.
Once stabilized and discharged, Nguyen felt emotionally detached from her baby and was fine handing the infant off to anybody else — a symptom of PPD.
She wondered why no one ever discussed the physical aftermath of birth.
“You're supposed to wear a diaper for six weeks, very much like: You’re a cow. Just have the baby, that is your job, you know, like we're just cows to breed,” she said.
At Nguyen’s six-week follow-up, the OB/GYN announced that she was “cleared for sex.”
When she became pregnant with her second child, she elected for a scheduled C-section. This way, at least, she could have the continuity of care and medical attention to minimize the chance of traumatizing emergencies and triggering a sense of lack of autonomy.
Nguyen continues engaging in elective therapy to navigate the trials and tribulations of parenting, which can sometimes trigger obsessive compulsive disorder and the feeling of losing control.
Pushing for postpartum care before we need it
Kumar commented that unaddressed postpartum difficulties do not necessarily go away on their own. She said that her office often sees people still struggling with mental health symptoms years after their childrens’ births. She also said that having PPD once is one of the highest risk factors for having it again.
The journey has been long for Owoimaha-Church. “Nine years later is when I began to have the language and the framing to know what happened to me,” she said. She was only able to access a therapist she liked and trusted a couple of years ago when transitioning to her current role at EPIC.
Noting the maternal health resources available today, many of which have only coalesced over the past few years, Owoimaha-Church said that she has seen a lot of good local-level work being done in certain communities to provide perinatal care. She feels unsure whether this trend is translating to mass-level change yet.
“What if we integrated all of this? There is prevention that can be done,” Kumar said, pointing out how rigorous screening is now for physical birth risks such as gestational diabetes, which affects people half as much as PPDdoes.
“How do we create a safety net that birthing people can't fall through?” she asked, stating that risks of perinatal mood and anxiety disorders should be discussed by anyone encountering a pregnant person. She also said that the trauma of childbirth must be named, and that doulas should do this instead of normalizing trauma as a rite of giving birth.
Experts have cited perinatal healthcare — “wraparound” care (including mental health care) for women and their babies before, during and after birth — as a public health crisis.
Seah said birthworkers exist to fill in the care gaps in existing healthcare systems, and that the people who need them most are those who give birth in hospitals. She estimated that 80–90% of her clients give birth in clinical settings, adding that the turnover rate due to burnout among birthworkers is high.
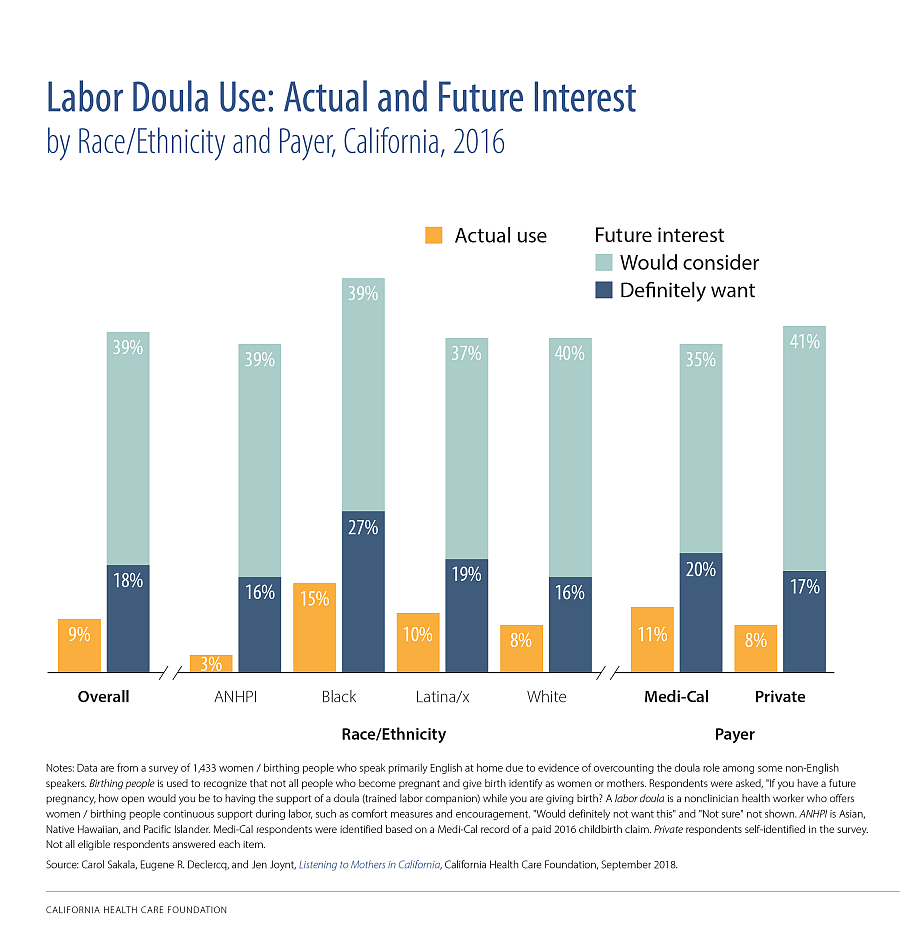
CHCF’s data also revealed that Asian and Pacific Islander people were the least likely of all groups to have used a labor doula before or want one and are among the least likely to consider doing so.
The National Health Law Program’s Doula Medicaid Project has been working to expand full-spectrum Medicaid coverage of doula care, including doula support during the prenatal and postpartum periods, labor/delivery, miscarriage, stillbirth and abortion.
As in Lim’s case, these doulas provide emotional support and relief and open doors to culturally competent specialists in physical recovery and mental health care who are in their networks.
In many more states, the systemic exclusion of these community-led solutions is written into law. In Hawai’i, HRS 457J, the attorney general’s clarification to the state’s midwifery laws that anyone giving maternal health advice or perinatal care could face fines and misdemeanors.
A Jan. 26 press release by the Pacific Birth Collective stated, “HRS 457 J criminalizes midwifery care that families already rely on.” This is especially the case in underserved, rural areas like the neighbor islands, where care is so scarce that birth emergencies can require a helicopter evacuation to Honolulu.
By contrast, at the beginning of 2023, California’s Department of Health Care Services (DHCS) began allowing doulas to be covered as a part of Medi-Cal.
A month ago, LAist evaluated the uptake. While Medi-Cal covered 168,000 births in 2021, 40% of the state’s births that year, only a fraction of Medi-Cal participants having babies in 2023 accessed doula benefits because of the administrative processes for doulas to become Medi-Cal providers.
“There’s a lot of catching up to be done,” Jasmine said.
Summers got mental health help in 2023, after divorcing her husband. She found a therapist who used to be an in-house specialist at a prominent comedy club. Soon thereafter, she quit drinking as her comedy and acting career ascended.
On a Sunday afternoon, roughly a year after only beginning her healing journey, she jumped with her children on a trampoline outside her home in Southern California before retreating to her dressing room.
Staring into a makeup mirror, she spoke of her Amazon comedy special currently in process, which centered around PPD.
“I think it's so important to talk about what’s going on, especially for the Asian American community. Because our older generation is just now believing in this,” she said.
She does not soften the harsh realities inspiring her humor advocacy for anyone — not even for her 4-year-old son.
He wants to be a comedian just like his mother.

Jiaoying Summers on the trampoline. Photo by Dustin McWethy
This AsAmNews project is supported by the USC Annenberg Center for Health Journalism, and is part of “Healing California,” a yearlong Ethnic Media Collaborative reporting venture with print, online and broadcast outlets across California.

