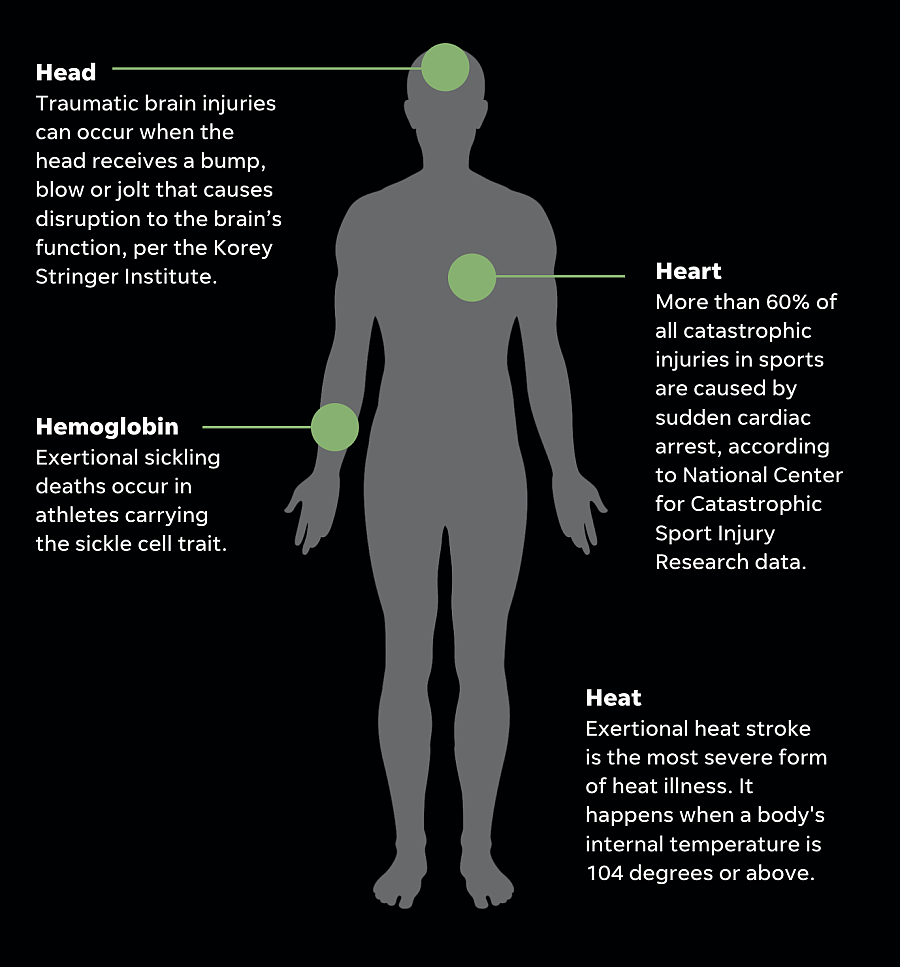
The 4 H's: The leading causes of death in high school athletes
The story was originally published in The Courier Journal with support from our 2022 Data Fellowship.
Sudden death in high school athletes happens every year.
And 90% of those are caused by one of four conditions: head, heart, heat and hemoglobin.
Expanded, those conditions look like catastrophic brain injuries (head), sudden cardiac arrest (heart), exertional heat stroke (heat) and exertional sickling (hemoglobin).
1. HEAD
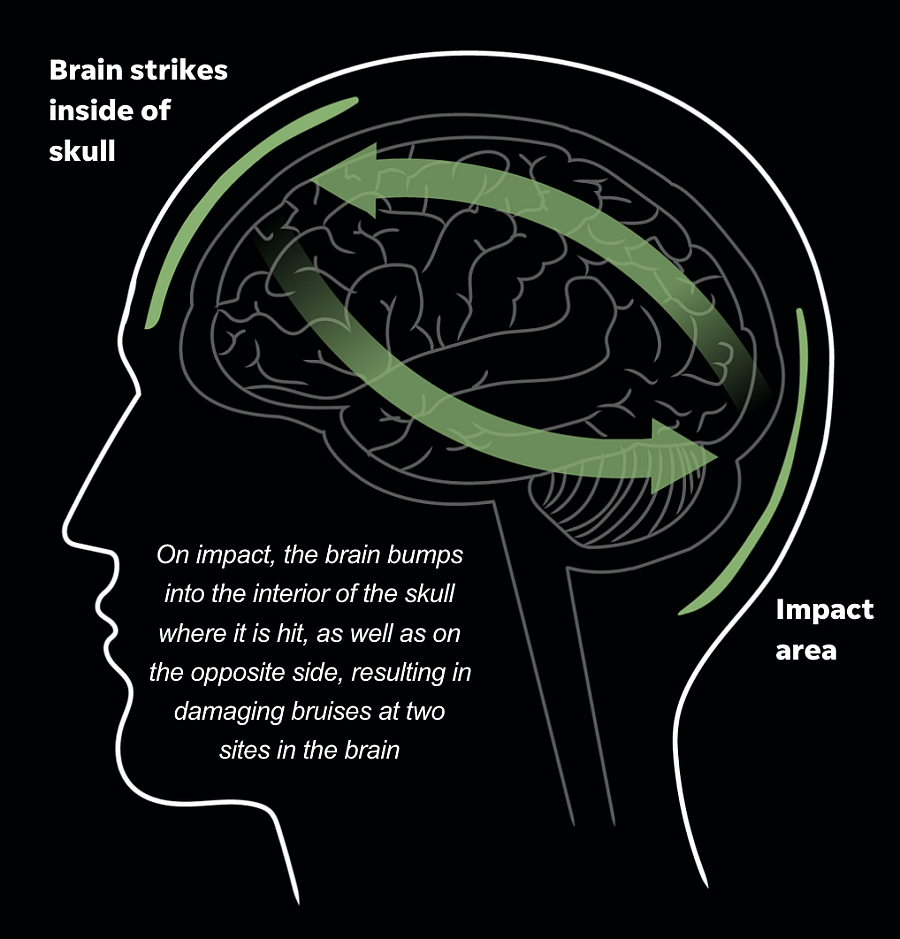
The most common type of head injury is a concussion, which creates dysfunctional processing caused by biomechnical forces.
The most deadly type is second-impact syndrome or when an athlete returns to play too soon after having a concussion and sustains another traumatic head injury.
Research says there are between 1.1 and 1.9 million sports and recreational related concussions in children 18 years or younger every year.
A concussion is usually the result of a blow to the head. This creates a mild bruising of the brain tissue.
There are generally three grades of a concussion, according to severity
- Grade 1
- Commonly referred to as a bell ringer. The player experiences confusion or inattentiveness for less than 15 minutes. There is no amnesia or loss of consciousness
- Grade 2
- Confusion is accompanied by other symptoms, such as ringing in the ears, amnesia and nausea.
- Grade 3
- A loss of consciousness.
Prevention
Preventative measure include:
- Properly fitted playing equipment
- Proper tackling techniques
- Enforcement of game rules
- Having on-site medical care and regulations
- Mandatory return-to-play criteria following head injures
Life-saving techniques
Recognition is key. A concussion can look like balance problems, blurred vision or dizziness, confusion or memory problems. An athlete that is concussed should be removed from play and evaluated by a doctor who clears them to play before returning to the field.
2. HEART
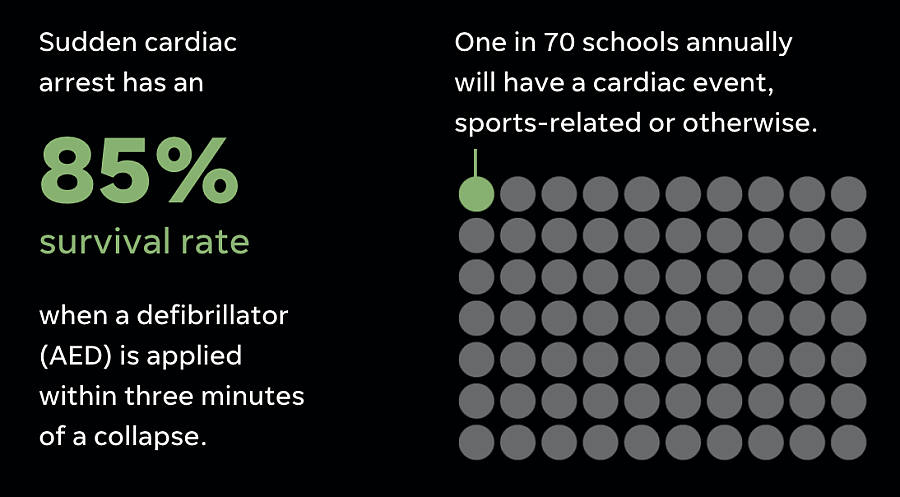
More than 60% of all catastrophic injuries in sports are caused by sudden cardiac arrest, according to National Center for Catastrophic Sport Injury Research data.
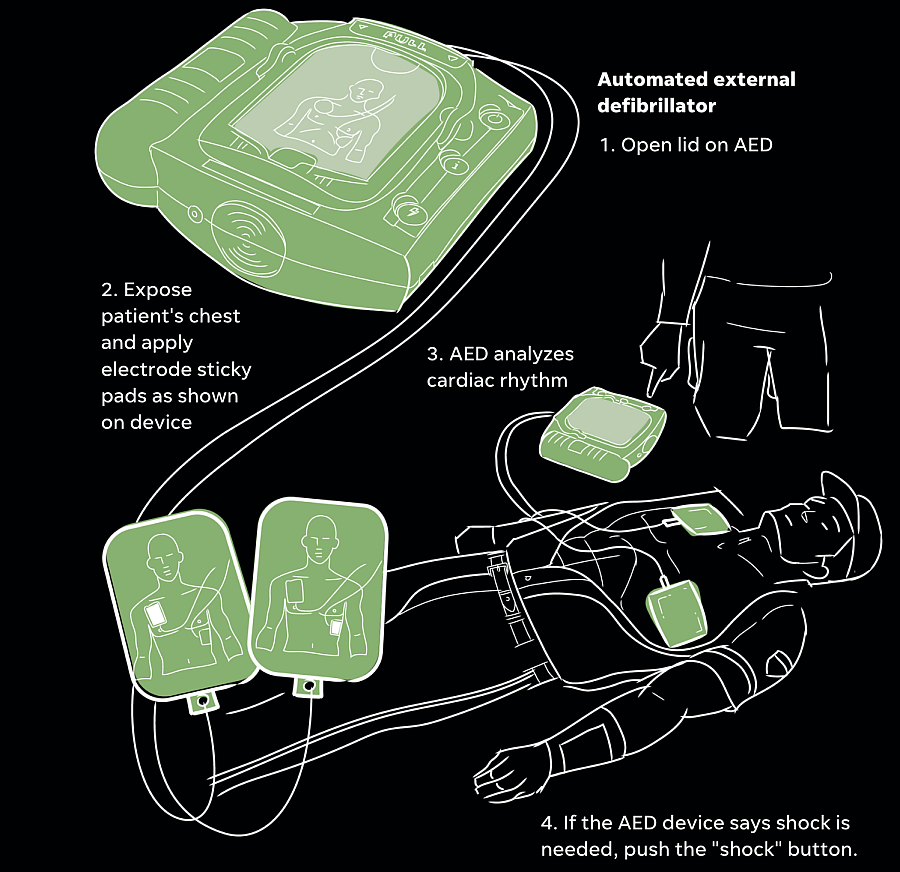
Life-saving techniques
When someone goes into cardiac arrest, it's a three step-process: call, push, shock.
CALL: When an athlete collapses, you will direct someone to call 911.
PUSH: Then you direct someone to grab the AED as you begin chest compressions, which can be done by interlocking your fingers and pressing the heels of your hand into the athlete's chest bone.
SHOCK: Once the AED arrives, apply the pads on the collapsed athlete's chest as instructed by the defibrillator.
Prevention
- Heart screenings like an echocardiogram that may detect a heart condition is just one prevention measure.
- Another is access to external defibrillators for those who have undetected heart conditions or may not have been screened. An AED can detect if a shock to a heart's rhythm is necessary.
- Sudden cardiac arrest drills involve running through an emergency response plan for who calls 911, who grabs the AED, where the AED is located, etc.
3. HEAT
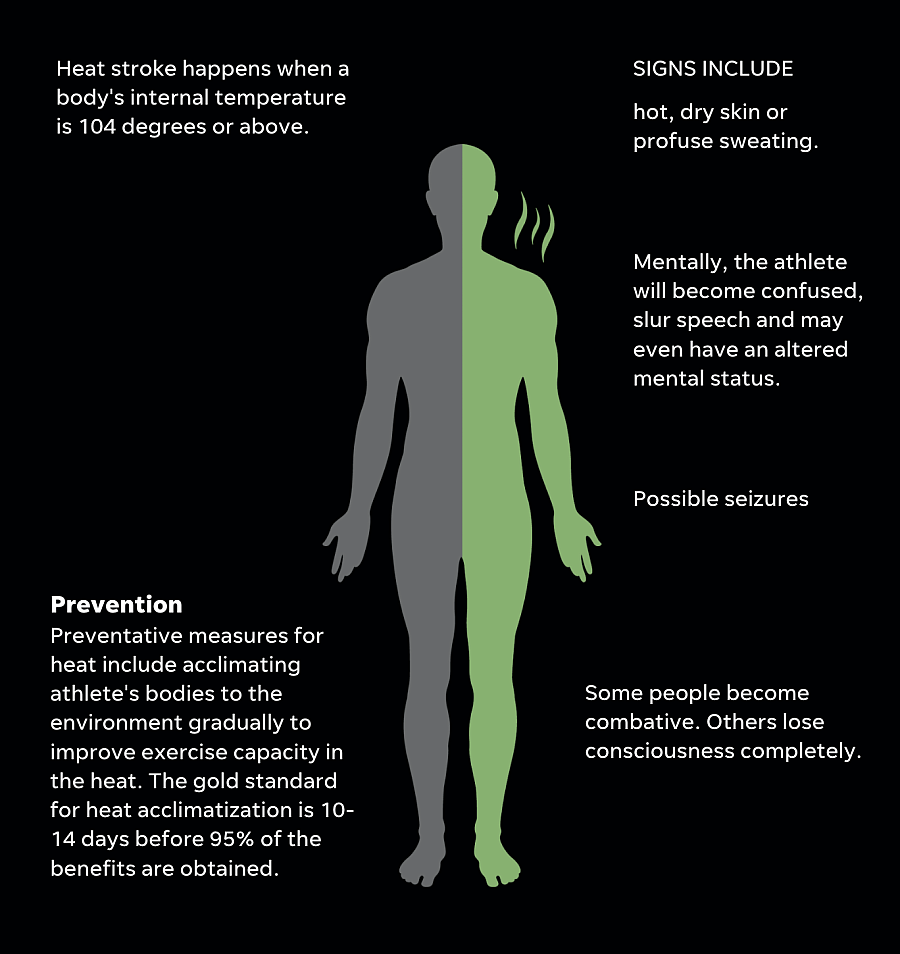
Exertional heat stroke is the most severe form of heat illness.
Life-saving techniques
- Cooling mechanisms are another preventative measure to combat the heat. Cold-water immersion tubs on sidelines during warm weather practices are considered best practice.
- If an athlete is believed to be having an exertional heat stroke, they should be cooled with cold-water immersion.
- There is a crucial window in which an athlete's temperature needs to be lowered, so it's important to lower the core temperature down to about 103 degrees as quickly as possible, usually within 10 minutes. That's why athletes should be cooled before they are transported by EMS. Think: Cool first, transport second.
4. HEMOGLOBIN
Exertional sickling deaths occur in athletes carrying the sickle cell trait.

Prevention
Preventative measures include screening athletes for sickle cell trait (a hemoglobinopathy panel), acclimating athletes with gradual increase of intensity when conditioning or lifting, limiting activity if an athlete with SCT is sick, educate athletes, parents and coaches on the signs and symptoms and treatment of exertional sickling.
Life-saving techniques
If someone sickles, the gold standard is to give them high-flow oxygen and nearly immediate IV access to get fluids starting to pump into their system. If none of that is possible, call 911 with an exertional sickling emergency.