Alaska doctor wheels hope to survivors of traumatic brain injury in his ‘Brain Bus’
The story was originally published by Alaska Beacon with support from our 2023 Domestic Violence Impact Fund.
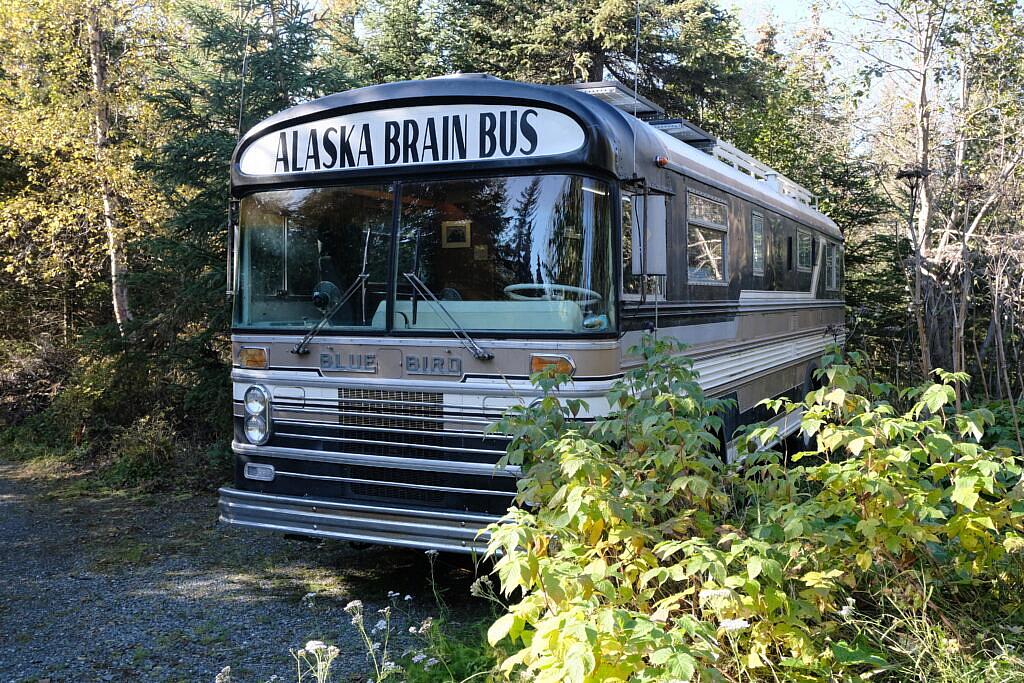
The Alaska Brain Bus is parked at Dr. Adam Grove’s South Anchorage home on Sept. 26, 2023.
Photo by Claire Stremple/Alaska Beacon
After a bike crash, Dr. Adam Grove noticed he wasn’t the same. He said he was depressed for the first time in his life, quick to anger and tired all the time.
It was 1998 and he was not yet a doctor, but had just left the military and begun medical school. He was commuting to class when the car hit him.
“At that time, nobody diagnosed the brain,” he said. “I was unconscious. I had broken bones and that kind of stuff, so they focused on that. Nobody said anything about brain injury. And so I muddled through medical school.”
He was not diagnosed with a traumatic brain injury until seven years later.

Dr. Adam Grove, seated in his Brain Bus, on Sept. 26, 2023.
Photo by Claire Stremple/Alaska Beacon
Alaska has the highest rate of traumatic brain injury in the nation; it is twice the national average. Medical providers say TBI is frequently undiagnosed or misdiagnosed, and that they need more training to do TBI screening, according to a state epidemiology report.
Now Grove is on a mission to increase awareness of traumatic brain injury, so people can treat it. His search for answers led him to years of advocacy, and eventually, to a bus.
With a grant from the Alaska Mental Health Trust, he converted a 1967 Blue Bird bus into a mobile medical office specifically for traumatic brain injury. He calls it the Brain Bus and drives from his home in South Anchorage to more remote locations on the road system to raise awareness about TBI and to counsel and connect people to resources.
“I can be the conduit”
Grove keeps the bus parked among some conifers at the end of a long drive in his wooded, South Anchorage neighborhood. It is his solution to what he described as a lagging response in statewide public health policy.
“We get so immersed in this whole policy thing. The problem is policies that never seem to trickle down to the people that I was working with,” he said. “So I decided to be the conduit.”
Instead, he is directly letting people know that they may have experienced a TBI and that help is available.
“I can sit with somebody and cry with them about the fact that their life is turned upside down and they’ve lost their families. Like, that’s useful,” he said.
You’re already at a disadvantage, and then add on a cognitive deficit. And it’s disastrous... It really hampers the decision-making process, which would enable them to exit the situation or to ask for help.
– Dr. Adam Grove, on the effects of traumatic brain injury in domestic violence situations
He described an 80-year-old woman who described years of struggle to get her injury and symptoms taken seriously.
“She said, ‘Every time I tried to get help and people told me, ‘There’s nothing wrong with you’ or, ‘Oh, you just hit your head,’ I’d just lose a little bit of confidence, and then a little bit more,’” he said.
And he said consequences from brain injury can quickly cascade into bigger problems, like homelessness. He said he has had patients who get brain injuries and lose their jobs because they cannot function at work. He said once the paychecks stop it can be a quick slide into homelessness.
“They can’t pay their rent, and within a month they’re living in their car. And then the car gets repossessed if they have payments on it. And now they’re homeless, right?” he said. “It’s easy, within a month or two.”
Nationally, about half of people who are experiencing homelessness also have a traumatic brain injury.
Brain injury and domestic violence
Grove does not keep track of how many people he has met on the bus, but he estimates that a third of the people he consults with have brain injury as a result of domestic violence.
“There is huge overlap,” he said, making the circles of a Venn Diagram of traumatic brain injury and domestic violence with his hands. The circles were nearly on top of one another.
He said most people with brain injuries are unaware they have them, which can be damaging because the symptoms can disrupt their lives, but he said it’s especially disruptive in situations of domestic violence.
“You’re already at a disadvantage, and then add on a cognitive deficit. And it’s disastrous,” he said. “It really hampers the decision-making process, which would enable them to exit the situation or to ask for help.”
He also pointed to growing evidence that brain injury can come from emotional abuse, too. He said there are imaging studies that show that verbal and emotional abuse can alter the way the brain develops. “That sounds like a brain injury — something that happens after birth, that alters the way the brain works,” he said.
Screening as prevention
Grove said that brain injuries can be treated, so it is important to catch them. He said he really wants to see more screening for brain injury early, before consequences like job loss, homelessness or justice involvement can cause irreversible damage.

The Alaska Brain Bus is parked in South Anchorage on Sept. 26, 2023.
Photo by Claire Stremple/Alaska Beacon
“Somebody runs into mental health, behavioral health and juvenile justice — screen them for brain injury! Right? Stop it before it becomes a thing,” he said.
He said one of the biggest challenges to getting treatment is knowing that a brain injury is the cause of symptoms.
That is where the bus comes in — with medically trained staff that are experts in brain injury, armed with resources for individuals and ready to help build solutions with communities that recognize their importance.

