Navigating Mental Health Care In and Out of Prison
The story was co-published with Black Voice News as part of the 2024 Ethnic Media Collaborative, Healing California.

Graphic created by Aryana Noroozi
Although Jorge Arturo Ruiz, 49, known as Arturo, showed signs of bipolar disorder throughout his life, he wasn’t diagnosed until he served a six-and-a-half-year prison sentence for domestic violence and great bodily injury. Arturo, now a resident of Moreno Valley, entered prison in 2017. He is one of roughly 37,000 incarcerated people who experienced a mental health condition while serving time in California state prisons.
Over the past decade, the number of incarcerated individuals in California jails with an active mental health case has risen by 63%, according to the California Department of Health Care Services (DHCS).
An estimated 18% of the general population has a mental health condition, while that proportion jumps to more than 37% for those in prison according to an analysis by the California Budget and Policy Center. This is true across the full spectrum of diagnoses, including bipolar disorders.
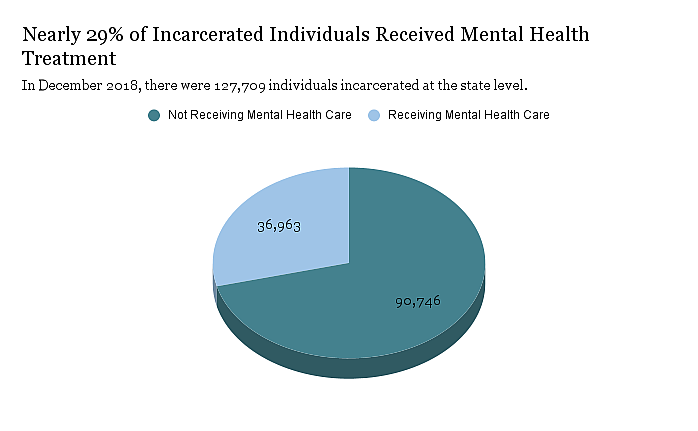
Nearly 29% of incarcerated individuals at the state level received mental health treatment in December 2018 according to an analysis of California Department of Corrections and Rehabilitation and the Department of Finance by the California Budget & Policy Center.
Data graphic by Breanna Reeves
According to the National Institute of Mental Health (NIMH), bipolar disorder is a mental illness that causes unusual shifts in a person’s mood, energy, activity levels, and concentration. These shifts can make it difficult to carry out day-to-day tasks due to clear changes in mood, energy and activity levels.
“It affected my relationships before prison. It affected my business’ success. I would make a lot of people mad and I would lose business,” Arturo said. “I lost a lot of good quality employees because of my bipolarity.”
The NIMH reports that these moods range from periods of extremely “up,” elated, irritable or energized behavior, known as manic episodes, to very “down,” sad, indifferent or hopeless periods, known as depressive episodes.
While completing his sentence at Corcoran State Prison, Arturo saw a therapist monthly and a psychiatrist regularly. But since his release just over a year ago, Arturo has had difficulty finding an adequate psychiatrist and therapist. Arturo finds this period of reintegrating into a new life after prison challenging and a time that is critical to maintain access to mental health treatment.
Arturo’s story sheds light on the complex dilemmas faced by many incarcerated or formerly incarcerated individuals who entered the system with preexisting mental health conditions and had to navigate mental healthcare while in prison. The struggle to access quality mental health care is ongoing as Arturo works to rebuild his life.
How childhood experiences impact mental health
Arturo was born in Los Angeles, but after his father left, his mother moved the family back to Mexicali where they lived with her parents and siblings. She worked most of the time and dated often.
“I would meet a new boyfriend every other weekend. So, I guess it was a very psychologically disturbing and abusive environment,” he said.
Arturo recalled his mother sending him out to sell ice cream with a cart on the street. He remembers what it felt like to dodge speeding cars and to be beaten by gangsters who sometimes stole his money.

Arturo attends his godson’s (right) first communion in 2012. He was 37 years old and had not begun using cocaine or excessively drinking alcohol at this time.
Photo courtesy Arturo Ruiz
According to a 2020 research study which examined more than 2,000 adults with bipolar disorder, different adverse childhood experiences (ACE) can have varying impacts on patients diagnosed with bipolar disorder. Adverse childhood experiences (ACE) are potentially physical, emotional or sexual traumatic events that occur in childhood.
The study found “a positive association between substance misuse and ACEs, which remained even after adjustment for sex and age. In addition to ACEs, being male was associated with an increased frequency of substance abuse or dependence.”
The authors found that 63.1% of the patients had a history of exposure to at least one ACE. They also noted that the more exposure to numerous ACEs had a significant association to the severity of clinical symptoms such as suicide attempts and multiple conditions related to substance misuse.
As Arturo grew older, he didn’t understand the highs and lows he experienced. He began to mask and self-medicate in the years leading up to his case. According to the NIMH, many people with bipolar disorder also struggle with substance abuse.
For Arturo, drinking and substance use became a way to numb the pain.
“After I became an alcoholic… I started doing coke and I fell in love with her. Once I did the first hit, I wasn't bipolar anymore. I was just happy the whole time, and every time I started to feel a little bipolar, I would just do another hit.”
Arturo attributes his substance abuse to putting himself in a predicament that led to his arrest.
An analysis of post-release care by Judi Nightingale, director of Population Health in Riverside County, highlighted the correlation between mental health attributes and recidivism. The report noted that 25% of incarcerated people with a mental health illness had three or more prior convictions compared to 5% of those without a mental health condition.
After serving time, Arturo was released into what he described as a new world.
“I come out — there’s no car, there’s no house because I got rid of everything and there’s really no money coming in,” he said.
“Mental illnesses are either the primary reason or a significant contributing factor to the reason they’re intersecting with the criminal justice system,” said Monica Ngyuen in a previous interview. Nguyen is a Riverside County deputy public defender and member of the mental health court.
She explained that the same reasons her clients couldn’t access mental health treatment prior to their alleged offense do not simply disappear once they enter the system. Consider someone who is self-medicating with drugs and now faces a drug charge, Nguyen described. Their mental illness worsens as they struggle with their mental illness, substance use and potential jail time.
Accessing treatment while inside
Prior to being sentenced, Arturo’s mental health worsened. He wanted to go to trial, but was urged to take an eight month deal so that his daughter wouldn’t be sent to Child Protective Services since his ex-wife was also arrested and charged alongside him.
Arturo expected to go to fire camp in lieu of prison, but instead he received a longer sentence and was sent to prison. It was during this time that Arturo began to feel a heavy weight on his shoulders.
Over the course of his six-and-a-half-year sentence, Arturo spent time in seven prisons across California and one in Arizona. It wasn’t until the last stretch of his sentence that he received treatment. After picking a fight at Chuckawalla Valley State Prison in Blythe, he ended up meeting with a psychiatrist.
“I was suicidal and I was picking fights with the biggest guys to see if they would punch my ticket,” he said. The psychiatrist suspected that Arturo’s behavior was a sign of suicidal behavior.
The psychiatrist wrote a referral for Arturo to begin treatment, but it was months later, when he was transferred to Corcoran — where he spent his final 18 months in prison — that he received treatment. According to Arturo, the treatment remained consistent for the duration of his confinement.
The California Department of Corrections and Rehabilitation (CDCR) has specific criteria for those who need a referral for mental health treatment. According to their mental health services program guide, any incarcerated individual who demonstrates unusual or uncharacteristic behavior while committing a disciplinary infraction is eligible for a referral.
At Corcoran, Arturo saw a therapist monthly and was diagnosed with bipolar disorder.
“That’s when I started learning about my disorder and I started learning how to cope with things,” he said.
He was prescribed medication that helped him feel more calm.
“You’re always on edge. You’re always vigilant. You’re always watching your back,” he said, explaining how the medication allowed him to be less hypervigilant.
Any incarcerated individual can be referred for mental health services at any time and can be referred for evaluation by concerned staff members.
According to CDCR policy, those incarcerated may self-refer or be referred by any staff member for a review by a mental health clinician. Referrals can be made on an emergent, urgent or routine basis. In the case of emergent referrals, the patient must be under constant observation until evaluated. An urgent referral must be seen within 24 hours and a routine referral should be seen within five working days.
However, formerly incarcerated individuals shared that in their experiences, this time frame is not always honored.
Last year, Raymond Goins was released from a 28-year sentence for robbery of an inhabited dwelling with a firearm. Today, he works with Silicon Valley De-Bug, a community-based advocacy organization. He said self-referrals can take months to be considered, if ever followed up on. While serving time, Raymond self-referred multiple times, but on several occasions CDCR claimed they never received his referrals.
“In my opinion, the policies and practices that could help remedy this is basic accountability and compassion,” Goins said. “[Humanize] the individual that is requesting help and disregard the inherent bias that staff has towards [incarcerated people].”
Finding mental health support after release
“Connecting people to mental health services can improve their health, their wellbeing, their financial security, and also reduce the likelihood that they return to the justice system,” said Vikki Wachino, executive director and founder of the Health and Reentry Project. Health and Reentry Project is an organization working to make policy changes at the intersection of health and reentry by partnering with those on the ground.
The Public Policy Institute of California analyzed 12-years of data from California jails and reported that those who are incarcerated with mental health needs have increased over 12 years, from 20% in January 2010 to 53% in June 2023.
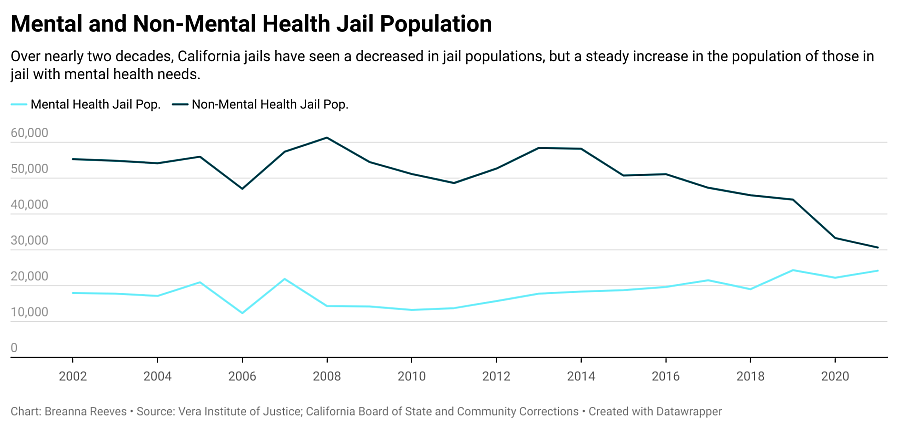
Across Riverside County, there are five jails and five county jails. According to data analysis by the Vera Institute of Justice, 38% of the jail population in Riverside had mental health needs in 2021.
As Arturo prepared for release from prison, exit counseling offered him little support when it came to coordinating mental health resources upon reentry.
Instead, Arturo was urged to reach out to the community. When it came to psychiatric care he described a “warm hand off” to a general psychiatrist. Once he was released, a physician began to call him once a month and ask if he is having suicidal thoughts and engaging in harmful or abusive behavior, then sent refills for medication.
“There is no, ‘How do you feel in the morning,’” Arturo shared. “He calls you from a blocked number and when you ask him for his email, he won’t give it to you and he won’t give you his number.”
While Arturo is confident he will be able to find adequate treatment, he worries for those who don’t share his level of education or resourcefulness. He’s concerned they will be “stuck” with inadequate treatment.
“They should be able to assign really good help so that you could thrive in your reentry process,” he said.
Nguyen explained that justice can be reformed if it is viewed as restorative.
“If you have that very narrow view of justice, you cannot reform,” she said. “Restorative justice is where you restore the defendant to a place where he or she can think straight or they can think straight. Therefore, they become a functioning member of society because they’ve gotten a handle on their mental illness.”
Gaps in resources during a critical time for support
Arturo has stopped taking the medications he was prescribed in prison. He doesn’t believe that he would be functional if he was still on the medications because they made him feel dull and depleted his memory.
“I don’t need to be sedated. I’m out here. I need to be functional, integrating myself into society,” he said.
Part of Arturo’s reintegration includes continuing his education. In 1998 he earned a bachelor of science degree in criminal justice from California State University, Los Angeles. In prison, he also took courses and upon release began studying history at Riverside Community College (RCC). Last semester he received Dean’s List honors and plans to attend a law program or obtain a master’s degree in business.
Arturo’s experience at RCC has been critical to his reentry process and mental health. He feels supported by the faculty and has access to necessary resources. But maintaining academic success coupled with working multiple jobs and volunteering in his community, under the constraints of parole, has not been easy.
Eliminating interactions with volatile people, from family members to former partners, has been a crucial yet difficult task. Arturo is currently renting a room in a sober living house with six other men whom he describes as dysfunctional.
“I’m under so much pressure that you don’t see. You just feel it like right here,” Arturo said, as he motioned to the base of his skull.
Coupled with frequent random visits from parole officers, working two to three jobs at a time and having his wages garnished for restitution, Arturo is juggling multiple stressors.
Over the past month, Arturo felt like he was close to a mental breakdown with the mounting pressures he faces.
The state’s solutions to improve continuation of care
In 2023 California was the first state to approve a targeted set of health services to youth and adults in state prisons, county jails and youth correctional facilities for up to 90 days prior to release, under California Advancing and Innovating Medi-Cal (CalAIM).
DHCS will partner with state agencies, counties, and community-based organizations to establish and coordinate a community reentry process. The program is intended to assist people leaving incarceration connect to the physical and mental health services they need prior to release.
A case study for the program depicted an individual being treated for bipolar disorder while in prison. It described how, through the initiative, he will be assigned a pre-release care manager who conducts a needs assessment and develops a reentry care plan to support his transition into the community.
Prior to release, he will also be connected to a psychiatrist in the community who will continue to care for him. This will start while patients are still in prison – through a “handoff meeting” between the patient, his correctional facility psychiatrist and his community-based psychiatrist. He will also receive a supply of his bipolar medication to take with him upon release. He will also be connected with Community Supports such as housing, to help him build stability in the community.
“Historically, people with mental health issues, who are leaving prison have struggled to connect to access services as they’re being released,” said Wachino. “Those changes could be life saving for people.”
However, Arturo’s release experience differs vastly from the hypothetical individual featured in the program’s case study. Arturo said it was unclear whether he was assigned a case manager during his reentry process. Instead, he recalled a CDCR staff member providing him with release documents. A week before he was released, Arturo’s parole conditions were changed to exclude him from residing in Los Angeles County after he had already made plans to live there. He had no choice, but to find accommodations in Riverside County without any housing from CDCR.
The Medi-Cal Justice-Involved Initiative is intended to close gaps in connecting incarcerated and newly released individuals with health care services. While the initiative received approval in January 2023, DHCS announced that they will delay the initiative from April 1, 2024 to October 1, 2024 to allow partnering agencies to better prepare for the two-year implementation period.
Every year, an estimated 35,000 people like Arturo are released from California prisons. The question of what resources are readily available and accessible during their reentry process remains unclear.
This Black Voice News project is supported by the USC Annenberg Center for Health Journalism, and is part of “Healing California,” a yearlong Ethnic Media Collaborative reporting venture with print, online and broadcast outlets across California.
