Dallas-Fort Worth lags behind other Texas cities in early blood transfusion care. But that's changing.
The story was originally published by the The Dallas Morning News with support from our 2022 National Fellowship.

Trauma nurse Kathrine Lozano administered a unit of blood to a patient in April at John Peter Smith Hospital in Fort Worth. John Peter Smith is a Level I trauma center for Tarrant County and surrounding areas.
Smiley N. Pool
Blood seeped from the stab wound in the man’s leg while paramedics tried desperately to revive him.
By the time trauma staff at Parkland Health pulled off his boots, a breathtaking amount of blood gushed out. The gash would have been simple to repair, had the weapon not sliced through his femoral artery.
Within minutes, he was dead.
Years later, Kristie Brown, the hospital’s director of trauma services and an advanced practice nurse, still thinks about that patient, about how he could have been helped by earlier access to a tourniquet or blood transfusions. What happened to him is a scenario she has observed time and again: Shooting and stabbing victims who were not far from her hospital when they were injured but arrived on the verge of death from massive blood loss.
Cases like his make her wish there was a way to get blood to patients before they get to the hospital, something that’s standard in some parts of Texas. But not yet in Dallas-Fort Worth.
In the fourth-largest metro area in the country with more than 7.5 million people, a combination of a complex network of health systems and sometimes competing interests have made medical leaders cautious about placing blood products on ambulances. That started to change after The Dallas Morning News began asking North Texas health leaders last year why blood programs were possible in some of the state’s other major cities but not here.
Aside from air ambulance companies, only three suburban EMS agencies across the region — in Frisco, Sachse and Parker County — provide blood products on ambulances. A fourth provider in Wise County, which includes Decatur, is on the cusp of carrying blood components.
The region’s two largest EMS providers, Dallas Fire-Rescue and MedStar Mobile Healthcare, which provides emergency medical services in Fort Worth and surrounding communities, said recently that they are in early discussions to carry blood products. While Dallas Fire-Rescue leaders said they intend to launch a pilot program in the first half of next year in partnership with Parkland Health, MedStar has no immediate plans to carry blood.
Local health care leaders argue that making blood products widely available across the region is complicated. With its size and sprawl, the Dallas-Fort Worth area has numerous competing hospital systems and EMS providers with varying need for blood and the ability to pay for it.
“I often will talk about the Metroplex being like three-dimensional chess,” said Rick Antonisse, executive director of North Texas’ regional trauma council.
Representatives at Carter BloodCare, the nonprofit blood bank that serves North Texas, are open to arming the region’s paramedics with blood products but have reservations about further straining an already limited blood supply and siphoning away units that hospital patients need. Dallas Fire-Rescue treats more than 160,000 patients each year, while MedStar responds to around 190,000 calls annually.
North Texas stands in stark contrast to San Antonio, Austin and other parts of South and Central Texas, where paramedics have routinely carried blood to scenes involving serious injuries and massive blood loss for years. Blood is one of the few tools paramedics can use to treat severe internal bleeding before a patient undergoes surgery.
These blood programs seek to address an intractable problem — the potentially preventable deaths of tens of thousands of injured patients annually who bleed out before they reach a hospital or soon after their arrival.
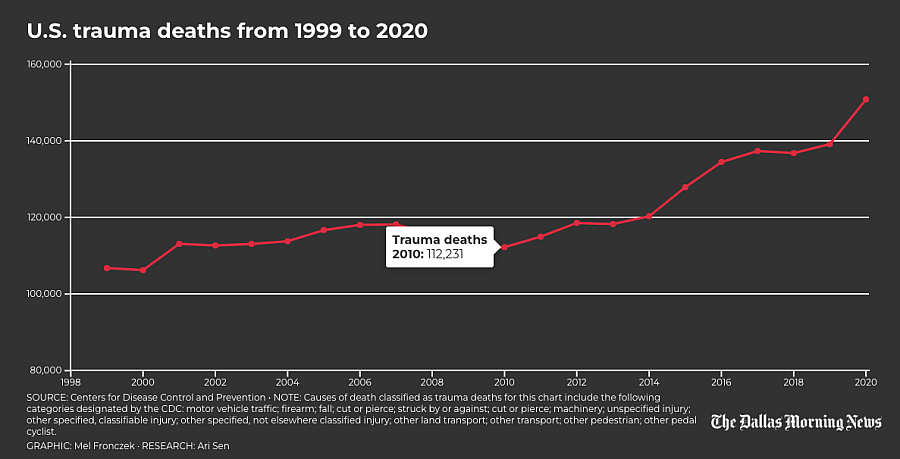
Trauma is the top cause of premature death for children and adults under age 45, and in 2021 Texas led the nation in deaths from motor vehicle crashes and guns, federal data shows. In 2020, traumatic injury killed an American about every 3½ minutes, a Texan every 42 minutes and a Dallas County resident every 7½ hours, according to the most recent data from the Centers for Disease Control and Prevention.
Each year, an estimated 31,000 injured patients bleed to death with potentially survivable injuries, which medical researchers say is a public health crisis. A significant share of these deaths could be averted with faster access to care, and in particular, blood, a growing body of research and an investigation by The Dallas Morning News and the San Antonio Express-News has found.
In Austin, paramedics immediately noticed the difference that rapid access to blood made for their patients, whether they were bleeding from a car crash, a gunshot wound, gastrointestinal issues or a pregnancy complication. To get blood to shooting victims sooner, Austin-Travis County EMS is training its paramedics to wear bulletproof helmets and vests so they can work alongside police.
“It became very apparent that this was a huge unmet need in EMS,” said Capt. Dave LeClere.
GALLERY: Austin EMS provides example for North Texas paramedics

Austin-Travis County EMS Commander Craig Smith(left) joined Austin firefighters as they extricated a patient from a motor vehicle accident in May. Blood is one of the few tools paramedics can use to treat sever internal bleeding at the scene of an accident.
Smily N. Pool / Staff Photographer

Smith helped firefighters as they loaded a patient for transport at the scene of a motor vehicle accident in May. In Austin, paramedics immediately noticed the difference that rapid access to blood made to their patients.
Smily N. Pool / Staff Photographer

Austin-Travis County EMS medics and Austin firefighters worked on a victim of a motor vehicle accident in the back of an ambulance in May. Unlike in North Texas, paramedics in Austin have routinely carried blood to accident scenes for years.
Smily N. Pool / Staff Photographer

A drop of blood falls from a finger as a paramedic with Austin-Travis county EMS stitched a lacerated finger at a patient collection point during SXSW festival.
Smily N. Pool / Staff Photographer

A police officer tried to wash away the blood at the scene after Austin-Travis County EMS took a patient from a downtown street during the SXSW festival. To get blood to patients who need it sooner, Austin Travis County EMS is training its paramedics to wear bulletproof helmets and vests so they can work alongside police officers.
Smily N. Pool / Staff Photographer

Commander Smith filled in the required paperwork on his phone for the blood he carried with him throughout his shift. Paramedics in Austin have carried blood to the scene of major accidents and shootings for years.
Smily N. Pool / Staff Photographer

Austin-Travis County EMS medics loaded a patient for transport at a patient collection point during the SXSW festival in March in Austin. In 2020, traumatic injury killed a Texan every 42 minutes, according to the Centers for Disease Control and Prevention.
Smily N. Pool / Staff Photographer

Austin-Travis County EMS units filled ambulance bays outside the emergency room as a patient was transported at St. David's South Austin Medical Center in May. Each year, an estimated 31,000 injured patients bleed to death with potentially survivable injuries, which amounts to a public health crisis, medical researchers say.
Smily N. Pool / Staff Photographer
The Houston Fire Department, one of the largest municipal fire agencies in the country, has secured initial funding for a blood program through a donation from the Fire Fighters Foundation of Houston, said Dr. Lars Thestrup, assistant medical director. One study found more than 130 trauma patients in Harris County died of potentially survivable bleeding in a single year.
“It’s heartbreaking for the paramedics to not be able to provide some care for that patient who’s bleeding out,” he said. “This is going to be a huge solution for them.”
In recent months, the North Central Texas Trauma Regional Advisory Council, which supports emergency medical services across the area, has said it is rolling out a pilot program that would make blood components more widely available to EMS providers.
The program’s goal is for five North Texas providers to start carrying blood products in 2024. The council plans to start accepting applications from eligible providers in January.
“I think, in time, North Texas will catch up,” said B.J. Smith, the blood bank’s vice president of operations.
EMERGENCY EXTRICATION
In Frisco, the idea for using blood in the field began at a construction site.
In early 2018, emergency responders converged at a neighborhood where single-family homes were being built. A construction worker’s leg had become tangled in the teeth of heavy machinery while he was digging a trench.
There was no saving the limb and no way to free him without inflicting further damage. Yet if they didn’t rescue him, and soon, he would die. A surgical amputation was the best option.
So, on that worksite, first responders assembled a makeshift hospital.
A surgeon from Medical City Plano performed the procedure. Paramedics from the Frisco Fire Department provided equipment, administered pain and sedation drugs and placed a breathing tube in the victim. An air ambulance brought blood components to the scene.
During the amputation, Dr. Mark Gamber, the fire department’s EMS medical director, had an epiphany.
His paramedics often started IVs and encountered patients with urgent bleeding. Why didn’t they always have blood with them?
At the time, no other EMS agencies in North Texas carried blood outside of helicopter services. They would be the first.
The idea had already gained traction in other parts of the state.
A Houston-area emergency provider had been carrying blood products to calls for two years, based on military evidence that replacing lost blood as soon as possible can save lives. The month before the amputation in Frisco, the same data had prompted trauma leaders in San Antonio to launch the country’s first regional blood program, an initiative that would make blood widely available on helicopters and ambulances across South Texas.
Paramedics in Frisco wanted to offer the same for their patients, who were 20 to 25 minutes from major trauma centers. For heavy bleeding, that was a long time to wait.
Throughout 2018, Gamber and others at the fire department sought advice from their peers in San Antonio and Harris County and discussed the idea with Plano’s trauma hospitals, which received the city’s most severely injured patients.
That December, a paramedic supervisor began carrying blood products less than a year after the amputation at the construction site.
One week later, they got their first opportunity to use them after another incident at a different construction site. This time, a fallen staircase had crushed a worker’s pelvis, causing major internal bleeding.
The paramedics gave him transfusions of red blood cells and plasma in the back of the ambulance. He fully recovered.
Still, it would take about four years for another North Texas ambulance service to launch a similar program.
BARRIERS TO BLOOD
Paramedics have traditionally not carried blood products because they are costly, supply is short and they have a limited shelf life. While putting blood products on ambulances has grown in popularity over the past few years, it is still a relatively new practice for both EMS providers and blood banks. Medical researchers still debate the type of blood products that should be used on ambulances and helicopters and the patients who stand to benefit the most from those transfusions.
These obstacles have slowed efforts to make prehospital blood widely available in North Texas.

Parker County Hospital District EMS field training officer Jordan Tolliver (right) exchanged units of blood with Craig Denny of Carter BloodCenter. Protocols to return blood nearing expiration to the blood center ensures that none of the precious commodity is wasted.
Smiley N. Pool / Staff Photographer
In 2020, Dr. Justin Northeim, assistant director of BEST EMS, which provides medical direction to EMS providers in North Texas and other parts of the state, approached Carter about supplying blood to two of his agencies. Sachse, north of Garland, and Parker County, west of Fort Worth, respectively had driving times of about 20 and 45 minutes from Level I trauma centers.
Northeim thought the idea would be fairly easy to implement because North Texas had an abundance of trauma hospitals, more than Houston, San Antonio or Austin.
He was not prepared for the roadblocks he faced over the next two years.
Representatives from Carter balked at the idea of supplying them with whole blood, which they did not stock in large amounts. Northeim could get blood from San Antonio’s blood bank, which already supplied units to EMS providers. But that was so far away they couldn’t easily return unused units, raising the risk of wasting blood.
Smith, the Carter representative, said the organization’s main concern is sustaining the blood supply, given how few people donate. Blood is needed more sporadically in the field than at hospitals, so there needs to be a plan for using the units elsewhere before they expire so they don’t go to waste, he said.
Eventually, the two sides reached a compromise.
Carter would supply red blood cells and plasma to the two EMS agencies and switch them out with fresh units before expiration. To help maintain the blood supply, the EMS providers would bring in three blood donations for each unit they received. People who donate on behalf of the EMS providers register with a special code.
After Parker County paramedics began carrying blood products, they treated a domestic violence victim with multiple stab wounds. The patient, who received blood products in the field and during air transport, made it to the hospital alive and ultimately recovered.
“She wouldn’t have survived, prior to blood,” Northeim said.

Dr. Justin Northeim, medical director of Parker County Hospital District EMS, donated blood at the Carter BloodCare Weatherford donor center. In 2020, Northeim approached Carter BloodCare about providing blood for two of his agencies with long drive times to trauma centers.
Smiley N. Pool / Staff Photographer
Up until recently, no one championed the idea of prehospital blood in North Texas, said Dr. S. Marshal Isaacs, medical director of Dallas Fire-Rescue and a professor of emergency medicine at UT Southwestern.
Carrying blood, especially in a big city like Dallas, requires resources and a reimagination of the role of paramedics in treating major blood loss, based on still-emerging evidence.
While there is some research linking prehospital blood programs to improved short-term survival for injured patients, researchers are still collecting data on how prehospital blood programs impact long-term survival in big cities, where ambulance transport times tend to be fast.
However, as more cities across the state and country have launched blood programs, Isaacs said fire department and city leaders now support providing that level of care for patients in Dallas.
“We don’t want to be first. We certainly don’t want to be last. We want to be best,” Isaacs said.
Before moving to Fort Worth, Dr. Jeff Jarvis tried to establish a blood program in Williamson County, which includes Round Rock and other communities north of Austin.
He encountered strict rules for monitoring the temperature of the blood to prevent it from spoiling, especially outside the highly regulated environments of hospitals. The same challenges temporarily grounded Austin’s blood program after its initial launch at the end of 2021.
Now, as chief medical officer of MedStar, which provides ambulance service for Fort Worth and 13 surrounding cities, Jarvis also has to contend with funding problems. The organization is working with the city of Fort Worth to identify ways to fill major revenue shortfalls, a problem afflicting EMS providers nationwide.
Jarvis and others in his organization are still committed to the idea of prehospital transfusion, including in big cities where research shows that injured patients still regularly bleed to death. Working out the details, including logistics and supply, will take time, he said.
In the meantime, he urged the public to do its part.
“Donate blood, please. The solution to this is in your body,” he said.
PILOT PROGRAMS
Dallas Fire-Rescue plans to launch its pilot blood program sometime during the first half of next year, after choosing an area of the city that sees high numbers of injured patients. Over time, the program will likely expand to include the entire city and may later include patients with major bleeding from medical complications, too, Isaacs said.
The program’s success will depend on the availability of blood, which Dallas Fire-Rescue hopes to source from Parkland, and training some portion of the department’s more than 900 frontline paramedics.
Funding will have to be worked out, too. The federal government and private insurers currently do not pay for blood transfused outside a hospital, although trauma advocates plan to petition for those rules to be changed.
In September 2022, representatives from Carter and the trauma council, which supports the area’s EMS providers, attended a seminar in San Antonio to learn more about the regional blood program there. Afterward, they formed a work group to explore creating something similar in North Texas.
It’s not as simple as copying the blood programs in other parts of the state, said Antonisse, the trauma council executive director. The Dallas-Fort Worth region has more trauma hospitals than other Texas cities and numerous EMS providers, each of which does things a bit differently, he said.
The group decided that any interested EMS providers must demonstrate their need for blood and ability to comply with the program’s requirements, including maintaining the blood, submitting data and bringing in more donors to the blood bank. The trauma council will purchase up to $8,000 of equipment for each participating EMS provider.
Over time, the blood program’s reach will expand, said Jim Dickerson, the council’s director of emergency health care systems.
“It’s not an unlimited, ‘Hey, everybody can jump in,’ ” Dickerson said.
That’s the very thing Carter is concerned about, he added.
HELPING BLEEDING PATIENTS
One afternoon this spring, a patient involved in a motorcycle crash, whose care was observed by a News reporter and photographer, reinforced the importance of having access to blood at a moment’s notice.
When the man arrived in the trauma bay of John Peter Smith Hospital, he seemed stable.
The patient, in his early 70s, had been airlifted to the Fort Worth trauma center after he was struck while riding his motorcycle in rush hour traffic. He had road rash on his face and torso and exposed bone on his arm and leg, but his vitals were strong.
Within a few minutes, he became incoherent, unable to answer nurses’ questions. Then his blood pressure fell sharply. Both were warning signs that he was bleeding out.
“Are we giving blood?” a nurse asked.
“Yes, one unit of blood, whole blood,” said Dr. Rick Miller, the hospital’s chief of surgery.

Emergency room workers crowded into a trauma bay at John Peter Smith Hospital in Fort Worth to assist in the treatment of a victim of a motor vehicle accident in April 2023. John Peter Smith is a Trauma Level I hospital.

A unit of blood was depleted as a patient was moved for more tests in the trauma center at John Peter Smith Hospital. The federal government and private insurers do not pay for blood that is transfused outside the hospital setting. Trauma advocates plan to petition for a change in those rules.

A trauma bay sat empty after a patient involved in a motor vehicle accident was given blood and then moved for more testing at Fort Worth’s John Peter Smith Hospital in April. X-rays showed the patient had a broken hip, which can lead to major internal bleeding.
Kathrine Lozano, a trauma nurse, weaved through the room, crowded with other nurses and flight paramedics, to a blue refrigerator stocked with four units of whole blood. They were kept within close reach for just this type of emergency.
As the blood began to flow, nurses ran an ultrasound to check for fluid in the man’s abdomen.
After a minute or two, the patient’s unintelligible garbling became clear responses. His blood pressure stabilized.
“All right, we’re going in the right direction,” Miller said.
X-rays showed the patient had a broken hip, which can lead to major internal bleeding.
For now, the blood had worked. Staff rolled him away for more tests.
John Peter Smith Hospital gives whole blood to revive hemorrhaging patients in its trauma bay because it’s faster and more potent than the combination of blood components patients typically receive. Dr. Raj Gandhi, trauma medical director, said the first time he gave it to an injured patient, it seemed to work like magic.
He also knows that what he can offer to patients at the hospital only partly addresses preventable bleeding deaths. For hemorrhaging patients, Gandhi said, the most important thing is quickly reversing the damage from massive blood loss.
Over the past 10 to 15 years, many trauma centers have begun to reach limits of what they can do to improve care for bleeding patients. That’s why Gandhi believes change needs to happen outside the hospital. He said he believes putting blood on ambulances and helicopters is the next frontier in saving more lives.
Gandhi wants to help all injured patients, not just those who make it to the hospital alive.